
Application of real-time shear wave elastography in the assessment of torsional cervical dystonia
Introduction
Cervical dystonia (CD) is the most common type of focal dystonia and characterized by abnormal head and neck movement and abnormal posture due to intermittent or persistent involuntary contraction of neck muscles, causing a significant physical and psychological burden or even loss of working ability (1). Botulinum toxin type A is still the treatment of choice for CD (2). In the anti-dystonia treatment, objective and accurate assessment of muscular tension and monitoring of muscular function is crucial for the treatment, efficacy assessment and guidance for further treatment.
In clinical practice, clinicians usually assess the affected muscles by clinical symptoms and palpation, but this is subjective. Electromyography (EMG) as an effective tool can aid the clinical assessment of affected muscle for clinicians (3,4). EMG can be divided into needle EMG and surface EMG, of which needle EMG has been widely used in clinical practice (5). Needle EMG can reveal the function and pathophysiological status of spastic neck muscles and contralateral antagonistic muscles, but the morphology of spastic and hypertrophic muscles cannot be identified. It is also invasive and may cause discomfort to patients (5). Surface EMG reflects the integrated myoelectric activity of muscles and is also non-invasive and easy to operate, but it cannot record the myoelectric activity of deep muscles and affected by some factors (6). Magnetic resonance elastography (MRE) is another method used for the assessment of spastic muscles and can detect muscular stiffness, but it is costly and time-consuming (7). Thus, it is necessary to develop non-invasive, intuitive, simple and convenient methods for observation of morphology, structure, and biology of muscles.
The muscular stiffness can objectively reflect the muscular status, and the spastic or twitching muscles have increased stiffness (8-10). Real-time shear wave elastography (SWE) is a new technique developed in recent years for measurement of tissue elasticity. This technique employs “Mach cone” principle and can collect the shear wave velocity by using ultra-fast imaging system for the calculation of elastic modulus of tissues, which can be used for the assessment of tissue stiffness. This technique has been a non-invasive, real-time, intuitive, simple and rapid one for assessment of muscular stiffness (11). It has been shown that SWE can be used for the measurement of shear elastic modulus of skeletal muscle (12-14). MSD stiffness was detected by using acoustic radiation force impulse in patients with congenital muscular torticollis (15). However, there was few studies reporting SWE applied in adult torsional cervical dystonia. In this study, (I) SWE was used for detection of shear elastic modulus of musculi sternocleidomastoideus (MSD) and musculi splenius capitis (MSC) in healthy controls; (II) the shear elastic modulus of MSD and MSC was compared between healthy controls and torsional CD (TCD) patients; (III) the relationship of shear elastic modulus of MSD and MSC with the degree muscular spasm determined by needle EMG parameters were assessed in CD patients. This study aimed to evaluate the value of SWE in the assessment of muscular status in TCD patients.
Methods
General characteristics
This study was approved by the Ethics Committee of Tongji Hospital of Tongji University. Written informed consent was obtained from each subject, and they understood the methods and examinations used in this study.
Patients with primary TCD were recruited from the Department of Neurology, Tongji University between March 2016 and March 2018, of whom simple TCD patients were recruited. Inclusion criteria were as follows: (I) patients were diagnosed with primary TCD; (II) simple TCD was confirmed. Exclusion criteria were as follows: (I) there were evident causes of TCD (such as brain trauma, spinal cord lesion, trauma, toxicity, perinatal injury, long term use of neuropsychiatric drugs); (II) there were comorbidities such as neurological diseases and systemic diseases; (III) there were nervous system positioning signs or cranial MRI showed abnormalities; (IV) patients received cranial or cervical surgery before recruitment; (V) patients received neck BTX-A treatment within the prior 3 months; (VI) patients were diagnosed with mixed TCD or simple TCD accompanied by continuous tremor.
In addition, healthy controls were recruited from the Center for Physical Examination of Tongji Hospital. There was no history of heart disease, diabetes mellitus, respiratory diseases, mental diseases, muscular dystrophy or head and neck pain in these patients.
Instrument and methods
Ultrasonography
SWE was performed by using the Aixplorer US system (SuperSonic Imagine, Aix-en-Provence, France) with an SL15–4 multifrequency linear probes operating at 4–15 MHz. MSD was superficial; thus the gen pattern was used in the general mode. MSC was relatively deeper than MSD, and superficial fascia was relatively compact. Thus pen pattern was adopted. The “penetration” mode was selected to deepen the penetration of the shear waves. The depth was 3 cm.
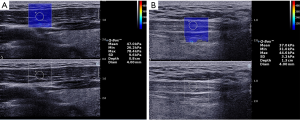
Patients were asked to sit on a chair with back leaning on the chair back. The neck was examined under pathological status, and patients should avoid the correction of head position. Some actions could induce pathological status. The probe was gently placed on the lateral neck to visualize the MSD with the depth of 3 cm and the elastic modulus of 0–600 kPa. On the cross-section, the thickness of MSD was measured at the middle of MSD. The MSD was examined along with the longitudinal axis up to the thoracic head and clavicular head. After examining the parallel muscle bundle, the examination was performed at elastography mode, and the lesion was determined in the area with the highest elastic modulus (Figure 1A). The region of interest (ROI) (10 mm × 10 mm) was determined, and the probe was maintained for several seconds. When the images became stable, the images were frozen, and round regions (diameter: 4 mm) were selected for the measurement of shear elastic modulus. The measurement was repeated 5 times. The system would automatically calculate mean Young’s moduli, MaxYoung’s moduli, minimum Young’s moduli of muscle in the region of interest, while mean Young’s moduli were used for statistical analysis. In the examination of MSC, the probe was placed on the back neck, and the MSC was examined from the linea nuchae superior to the spinous process of a fifth cervical vertebra. The thickness of MSC was measured on the cross-section. After examining the parallel muscle bundle along the longitudinal axis from the seventh cervical vertebra to the linea nuchae superior, the lesion was determined at the region with the highest elastic modulus (Figure 1B). The measurement was repeated 5 times, and a mean was calculated. The shear elastic modulus of MSD and MSC was also examined in controls with similar methods. Because the severity of lesions at upper, middle and lower part of MSD and MSC were different in CD patients, indicating that sometimes lesions focused at a specific segment, the muscular stiffness of upper 1/3, middle, and lower 1/3 part of MSD and MSC were usually detected, the maximal stiffness was chosen as ROI, and elastic modulus was measured. Meanwhile, the results of elastic modulus and electromyography were run for correlation analysis. During the examination, pressure should not be administered via the probe, and examination was done in the same room at the room temperature of 24 °C by the same physician who had a 10-year experience on the ultrasound examination of skeletal muscles.
Exploration by needle EMG and infusion after localization
Subjects were asked to achieve good rest on the day of examination. In addition, oral drugs (such as Baclofen, clonazepam, benzoresin hydrochloride, etc.) and excitatory nerve drinks (such as wine, coffee, tea, etc.) were discontinued on the day of examination. In this study, electromyograph and evoked potential detector (NTZ-2000, Shanghai Nuocheng Electric Co., Ltd.) were used. Patients were asked to sit on a chair, and the examiner stood beside or back of the subject. Electrode placement: generally, the electrode was placed at the detection site and injection site. Localization of the muscle: the head turned to the opposite side, and the needle was placed at the upper, middle, thoracic head and clavicular head of the muscle, followed by EMG at 2–5 points; the skin and muscle were fixed with a hand of the examiner, and then the needle was inserted into the MSC, followed by EMG at 3–6 sites. Diagnostic criteria: subjects were asked to relax or keep the neck at the abnormal status. The involvement of the examined muscle in the abnormal movement was determined according to the motor unit action potential (MUAP) measured by EMG. The cluster release of EMG signals with the rhythmic sound of released action potential on EMG suggested the involvement of the muscle in the abnormal neck movement (16). After examination, Botox injection was performed once the involvement of the muscle was confirmed.
Statistical analysis
All the data are expressed as mean ± standard deviation and statistical analysis were performed with SPSS version 21.0. In this study, continuous variables (such as body weight, BMI, shear elastic modulus, muscular thickness) were compared with the independent t-test, and correlation analysis was done with the Pearson correlation analysis. Categorical variables (such as gender, left/right handedness) were compared with independent Chi-square test, and correlation analysis was done with the Spearman rank correlation test. A value of P<0.05 was considered statistically significant.
Results
General characteristics
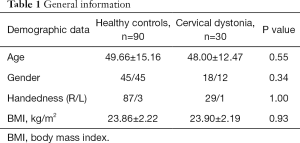
Among these 120 patients with primary CD, 33 patients were diagnosed with simple TCD, and finally, 30 patients received ultrasound examination of the muscles after exclusion of 3 patients with continuous tremor. Right torsion was found in 18 patients, left torsion in 12 patients, and 11 patients had concomitant should elevation. The longest course of disease was 125 months, and the shortest one was 1 month (mean: 29.27±31.55 months). According to the Tsui scale (17), the score of these patients was 3–10 (mean: 6.47±2.76). The spasm mainly involved ipsilateral MSC, musculi levator scapulae, contralateral MSD, and cucullaris. 90 healthy controls were divided into 3 groups according to the age: 20–39 years group, 40–59 years group and 60–79 years group (n=30 per group). The age, gender, BMI and handedness of subjects are shown in Table 1.
Full table
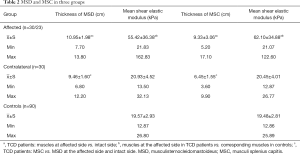
In 7 patients, the shear elastic modulus was undetectable due to thick MSC. In TCD patients, the thickness of affected MSD was 1.49±1.53 cm thicker than that of intact MSD (max: 6.10 cm) (P<0.01); the thickness of affected MSC was 2.87±2.67 cm thicker than that of intact MSC (range: 0.10–8.70 cm) (P<0.01). In addition, the thickness of affected MSC and MSD in TCD patients was also significantly different from that in controls (P<0.01). The elastic modulus was comparable between MSD and MSC (P>0.05). The elastic modulus of intact MSD and MSC in TCD patients was also similar to that in controls (P>0.05). SD value was relatively high in the affected group, which was associated with disease severity according to Tsui scale. The difference of Young's moduli between severing and the mild lesion was big, leading to high SD value with a maximum >30 kPa, while the difference of mean Young's moduli in normal muscle tissues, leading to low SD value with a maximum >4 kPa (Table 2).
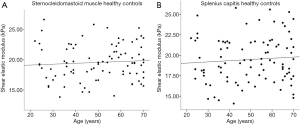
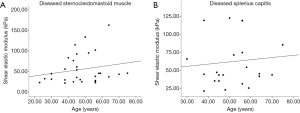
In healthy controls, the shear elastic modulus of MSC and MSD had no
Full table
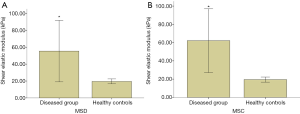
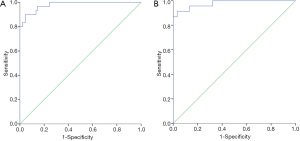
The elastic modulus of affected MSD and MSC in TCD patients was significantly different from that in healthy controls (P<0.01) (Figure 4). ROC analysis showed the diagnostic threshold of MSD and MSC was 24.90 kPa and 25.07 kPa, respectively (area under ROC: 0.979 and 0.979; sensitivity: 90.0% and 91.3%; specificity: 95.6% and 96.7%) (Figure 5).
The intraclass correlation coefficient of MSD and MSC elastic moduli in the normal control group was 0.92 and 0.91 respectively. The intraclass correlation coefficient of contralateral MSD and MSC elastic moduli was 0.90 and 0.91 respectively. The intraclass correlation coefficient of affected MSD and MSC elastic moduli was 0.89 and 0.88 respectively (Table 3).

Full table
Discussion
TCD is the most common type of CD (18) and mainly involves contralateral MSD, cucullaris, ipsilateral MSC and musculi levator scapulae. Especially, the MSC and MSD are the most susceptible to CD (18). Thus, in the present study, MSD and MSC were examined by SWE, and the shear elastic modulus of both muscles was determined, aiming to assess the features and muscular tension of both muscles in TCD patients.
The cause of CD remains still poorly understood (19). It has been widely accepted that the occurrence of CD is as a result of interaction between genetic and environmental factors. In the early phase of CD, the spastic muscles have weak strength and the corresponding contralateral muscles may counteract with it, and thus there is no significant difference in the muscular volume. The progression of CD may significantly increase the difference in the muscular strength between the intact side and affected side. The volume of spastic muscles may progressively increase due to the long-term uncontrollable movement, resulting in hypertrophy and stiffness of affected muscles. There is evidence showing that the distribution of spastic and hypertrophic muscles on CT is closely related to the type of CD (20). Generally, the hypertrophic muscles are mainly distributed in the posterior 1/4 region of rotator capitis side (such as MSC, musculi semispinalis capitis, musculus semispinalis cervicis, and musculi levator scapulae). In the present study, routine ultrasonography was done to measure the thickness of related muscles. Currently, there is no normal range for neck muscles on the cross-section. Thus, it is crucial to compare the muscles of both sides. Our results showed the thickness of spastic muscles increased significantly as compared to corresponding contralateral muscles in TCD patients, and the increase was more evident in the MSC of rotator capitis side.
As compared to other elastographic techniques, SWE does not require manual compression, which reduces the operation error and increases the repeatability (21-23). In addition, it determines the shear elastic modulus which represents the biological characteristic of muscles, and thus it is applicable in the quantification of muscular tissues. Examiner intraclass repetitive researches were also conducted in this study. Results showed that ICC was over 0.75, indicating that elastic moduli measure with SWE was reliable and repeatable. Muscular tissues have anisotropy. It is speculated that during the measurement of shear elastic modulus, the measurement will be more accurate and have better repeatability when the acoustic beam plane is parallel to that of muscular fibers (24). In the present study, the probe was parallel to the muscular fibers in the measurement of MSC and MSD. SWE can quantify the shear elastic modulus of neck muscles in a non-invasive manner. Our results showed there was a significant difference in the shear elastic modulus of MSC and MSD between healthy controls and CD patients, and the diagnostic threshold was 24.92 and 25.22 kPa, respectively, with high sensitivity and high specificity. In our study, the subjects were asked to keep calm during the measurement because MSD was superficial, and thus the results were stable. However, the elastic modulus of MSC was undetectable in 7 subjects. This might be ascribed to that the MSC is deep (under the cucullaris), the muscles in back neck became thicker, and the vibration amplitude of tissues in back neck reduces because the connective tissues in the back neck are dense and the probe frequency is limited (4–15 MHz). In the present study, only simple TCD patients were included, and those with continuous tremor were excluded because our previous findings showed the shear elastic modulus on SWE was unstable in patients with continuous tremor.
Arda et al. (25) speculated that the mean elastic modulus of normal masseter, gastrocnemius, and supraspinatus had no relationship with age, and there was no significant difference in the elastic modulus among different muscular tissues. Our results showed the shear elastic modulus of affected MSD and MSC in TCD patients, and that of MSD and MSC in healthy controls had no relationship with age, and there was no significant difference in the shear elastic modulus between MSC and MSD in healthy controls.
Nordez et al. (26) applied SWE in the assessment of shear elastic modulus of musculus biceps brachii during the isometric contraction, and results showed the shear elastic modulus was positively related to the myoelectric activity during the isometric contraction and linearly associated with the myoelectric activity in a specific range of isometric contraction. Our results showed the elastic modulus of spastic muscles was significantly higher than that of contralateral muscles, which suggests that the stiffness of affected muscles is higher than that of intact muscles. In addition, it was positively related to the myoelectric activity on needle EMG.
There are still several limitations to this study. Although the patients were blind to examination, the double-blind examination was difficult for the examiner, which may cause bias in the explanation of results. Moreover, the sample size was small, and a single center was involved, which may cause subjective errors. Thus, our results should be further validated in more multicentered studies with large sample size.
Taken together, SWE is a simple and convenient method for the assessment of muscular strength. The measurement of muscular mechanical properties is helpful for the understanding of the interaction between muscular structure and function, and for quantification of muscular elasticity, which provide scientific evidence for the diagnosis of spastic muscles and following assessment of prognosis. Thus, SWE has applicable good value in clinical practice. Of note, there are several limitations to SWE which is also muscle selective, and more clinical trials with large sample size are warranted to confirm our findings.
Acknowledgements
Funding: This study was supported by the Building Project of Clinical Assistant Department Capacity of Shanghai Shenkang Hospital Development Center (No. SHDC22015009).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was conducted in accordance with the Committee for Human Research at our institution and followed all regulations. Informed consent was obtained before scans.
References
- Jankovic J, Leder S, Warner D, Schwartz K. Cervical dystonia: clinical findings and associated movement disorders. Neurology 1991;41:1088-91. [Crossref] [PubMed]
- Simpson DM, Blitzer A, Brashear A, Comella C, Dubinsky R, Hallett M, Jankovic J, Karp B, Ludlow CL, Miyasaki JM, Naumann M, So Y. Assessment: Botulinum neurotoxin for the treatment of movement disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2008;70:1699-706. [Crossref] [PubMed]
- Delval A, Krystkowiak P, Cassim F, Skrzypzak L, Destee A, Derambure P, Defebvre L. Rev Neurol (Paris) 2004;160:547-53. [Usefulness and limitations of polymygraphic recordings in dystonia]. [Crossref] [PubMed]
- Graham D, Aquilina K, Mankad K, Wimalasundera N. Selective dorsal rhizotomy: current state of practice and the role of imaging. Quant Imaging Med Surg 2018;8:209-18. [Crossref] [PubMed]
- Daube JR, Rubin DI. Needle electromyography. Muscle Nerve 2009;39:244-70. [Crossref] [PubMed]
- Chowdhury RH, Reaz MB, Ali MA, Bakar AA, Chellappan K, Chang TG. Surface electromyography signal processing and classification techniques. Sensors (Basel) 2013;13:12431-66. [Crossref] [PubMed]
- Debernard L, Robert L, Charleux F, Bensamoun SF. Analysis of thigh muscle stiffness from childhood to adulthood using magnetic resonance elastography (MRE) technique. Clin Biomech (Bristol, Avon) 2011;26:836-40. [Crossref] [PubMed]
- Fischer AA. Tissue compliance meter for objective, quantitative documentation of soft tissue consistency and pathology. Arch Phys Med Rehabil 1987;68:122-5. [PubMed]
- Morisada M, Okada K, Kawakita K. Quantitative analysis of muscle hardness in tetanic contractions induced by electrical stimulation in rats. Eur J Appl Physiol 2006;97:681-6. [Crossref] [PubMed]
- Yanagisawa O, Niitsu M, Kurihara T, Fukubayashi T. Evaluation of human muscle hardness after dynamic exercise with ultrasound real-time tissue elastography: a feasibility study. Clin Radiol 2011;66:815-9. [Crossref] [PubMed]
- Gennisson JL, Deffieux T, Mace E, Montaldo G, Fink M, Tanter M. Viscoelastic and anisotropic mechanical properties of in vivo muscle tissue assessed by supersonic shear imaging. Ultrasound Med Biol 2010;36:789-801. [Crossref] [PubMed]
- Aubry S, Nueffer JP, Tanter M, Becce F, Vidal C, Michel F. Viscoelasticity in Achilles tendonopathy: quantitative assessment by using real-time shear-wave elastography. Radiology 2015;274:821-9. [Crossref] [PubMed]
- Brandenburg JE, Eby SF, Song P, Kingsley-Berg S, Bamlet W, Sieck GC, An KN. Quantifying passive muscle stiffness in children with and without cerebral palsy using ultrasound shear wave elastography. Dev Med Child Neurol 2016;58:1288-94. [Crossref] [PubMed]
- Dubois G, Kheireddine W, Vergari C, Bonneau D, Thoreux P, Rouch P, Tanter M, Gennisson JL, Skalli W. Reliable protocol for shear wave elastography of lower limb muscles at rest and during passive stretching. Ultrasound Med Biol 2015;41:2284-91. [Crossref] [PubMed]
- Park GY, Kwon DR, Kwon DG. Shear wave sonoelastography in infants with congenital muscular torticollis. Medicine (Baltimore) 2018;97:e9818. [Crossref] [PubMed]
- Rubin DI. Needle electromyography: basic concepts and patterns of abnormalities. Neurol Clin 2012;30:429-56. [Crossref] [PubMed]
- Tsui JK, Eisen A, Stoessl AJ, Calne S, Calne DB. Double-blind study of botulinum toxin in spasmodic torticollis. Lancet 1986;2:245-7. [Crossref] [PubMed]
- Nijmeijer SW, Koelman JH, Kamphuis DJ, Tijssen MA. Muscle selection for treatment of cervical dystonia with botulinum toxin--a systematic review. Parkinsonism Relat Disord 2012;18:731-6. [Crossref] [PubMed]
- Hutchinson M, Isa T, Molloy A, Kimmich O, Williams L, Molloy F, Moore H, Healy DG, Lynch T, Walsh C, Butler J, Reilly RB, Walsh R, O'Riordan S. Cervical dystonia: a disorder of the midbrain network for covert attentional orienting. Front Neurol 2014;5:54. [Crossref] [PubMed]
- Li LC, Tang BH, He YQ. CT Manifestations and its Value in the Diagnosis of Spasmodic Torticollis. Radiol Practice 2008.
- Brandenburg JE, Eby SF, Song P, Zhao H, Landry BW, Kingsley-Berg S, Bamlet WR, Chen S, Sieck GC, An KN. Feasibility and reliability of quantifying passive muscle stiffness in young children by using shear wave ultrasound elastography. J Ultrasound Med 2015;34:663-70. [Crossref] [PubMed]
- Lacourpaille L, Hug F, Bouillard K, Hogrel JY, Nordez A. Supersonic shear imaging provides a reliable measurement of resting muscle shear elastic modulus. Physiol Meas 2012;33:N19-28.
- Rosskopf AB, Ehrmann C, Buck FM, Gerber C, Fluck M, Pfirrmann CW. Quantitative Shear-Wave US Elastography of the Supraspinatus Muscle: Reliability of the Method and Relation to Tendon Integrity and Muscle Quality. Radiology 2016;278:465-74. [Crossref] [PubMed]
- Miyamoto N, Hirata K, Kanehisa H, Yoshitake Y. Validity of measurement of shear modulus by ultrasound shear wave elastography in human pennate muscle. PLoS One 2015;10:e0124311. [Crossref] [PubMed]
- Arda K, Ciledag N, Aktas E, Aribas BK, Kose K. Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. AJR Am J Roentgenol 2011;197:532-6. [Crossref] [PubMed]
- Nordez A, Hug F. Muscle shear elastic modulus measured using supersonic shear imaging is highly related to muscle activity level. J Appl Physiol 1985;2010:1389-94. [PubMed]


