Coexistence of acute miliary pulmonary tuberculosis and metastatic lung adenocarcinoma: a case report
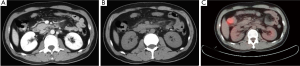
A 36-year-old man complained of cough, expectoration and progressive anhelation for more than three months. He was diagnosed with acute miliary pulmonary tuberculosis (AMPT) according to sputum culture of tubercle bacilli and CT scans (Figure 1A,B). However, symptoms didn’t alleviate after anti-tuberculous treatment for nearly one month. Subsequently, sputum cytology found a few lung adenocarcinoma cells and immunohistochemistry revealed it mostly came from intestinal duct. Moreover, glucose metabolism was increased at the whole lung field shown by PET/CT (Figure 1C). Furthermore, he described a history of mucus stool, without hematochezia, abdominalgia, diarrhea and abdominal distension. A large ulcerous neoplasm was found in the ascending colon by fibrocolonoscope. Adenocarcinoma of colon was finally confirmed by histopathology and PET/CT images (Figure 2).

To our best knowledge, the case described in this report is rare and valuable for its difficulty to diagnosis. Karnak et al. (1) reported 73 patients had coexistence of pulmonary tuberculosis (TB) and malignancy, in which lung cancer had the highest probability. It mainly exists in elderly people due to the relatively high incidence rate of both TB and malignancy. Karasawa et al. (2) reported the coexistence rate in elderly patients ranged from 1% to 2%. However, in our case, it was a young man who suffered it. Rybacka et al. (3) reported that tuberculous patients with little improvement of symptoms by anti-tuberculous therapy were not always caused by bactericidal resistance. In these cases, TB should be diagnosed cautiously, and lung cancer should be paid more attention. Conclusively, our initial diagnosis of AMPT was inaccurate because of cancer nodules masked by tuberculous lesions. We suggest that once miliary nodular shadows of lungs are observed, it is common to suspect TB at the outset, but the differential diagnosis of lung cancer also should be kept in mind.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Karnak D, Kayacan O, Beder S. Reactivation of pulmonary tuberculosis in malignancy. Tumori 2002;88:251-4. [PubMed]
- Kurasawa T. The coexistence of pulmonary tuberculosis and lung cancer. Nihon Rinsho 1998;56:3167-70. [PubMed]
- Rybacka-Chabros B, Mańdziuk S, Berger-Lukasiewicz A, et al. The coexistence of tuberculosis infection and lung cancer in patients treated in pulmonary department of Medical Academy in Lublin during last ten years (1990-2000). Folia Histochem Cytobiol 2001;39:73-4. [PubMed]


