Gadofosveset-enhanced magnetic resonance imaging as a problem-solving tool for diagnosing colorectal liver metastases: a case report
Introduction
Colorectal cancer is the second leading cause of cancer deaths in North America (after lung) (1). Most patients die of metastatic disease, usually to the liver (2). With significant advances in surgery and chemotherapy in the last few decades, the 5-year survival of patients with colorectal cancer in patients is 35% and is curative in up to 20% of patients (2). This is compared to a median survival of 7.5 months in untreated patients (3). Therefore, accurate per-lesion diagnosis of all colorectal liver metastases is crucial for surgical planning.
Detection of liver lesions is excellent with the use of magnetic resonance imaging (MRI) with hepatobiliary-specific contrast agents due to lesion conspicuity on hepatobiliary phase imaging; however, both hemangiomas and colorectal liver metastases are hypointense relative to the enhancing background liver making characterization difficult (4). Characterization of colorectal liver metastases is often done with MRI with extracellular contrast agents, but this remains limited, possibly due to delayed retention of contrast of some fibrotic liver metastases, which mimics benign hemangiomas (5).
It has been suggested that delayed retention of contrast is not seen in colorectal liver metastases on MRI with intravascular contrast agents such as gadofosveset; however, only four cases of colorectal liver metastases imaged with gadofosveset-enhanced MRI has been described in the literature (6,7).
This case report describes one case where gadofosveset-enhanced MRI was a helpful clinical problem-solving tool in a surgical patient with colorectal liver metastases.
Case presentation
We present a case of a 64-year-old woman who presented to an outside hospital with a 1-month history of lower abdominal pain. A computed tomography (CT) scan of the abdomen and pelvis revealed a locally advanced cecal mass with involvement of the abdominal wall. Colonoscopy revealed a large mass in the cecum and biopsies showed tubulovillous adenoma with high-grade dysplasia. She then underwent a colonic resection and pathology confirmed a T4N0 mucinous colonic adenocarcinoma.
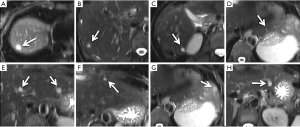
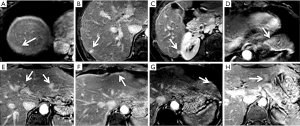
Postoperatively, she had a contrast-enhanced CT of the abdomen and pelvis and was noted to have multiple liver lesions. Based on the CT, all lesions were thought to represent multiple metastases. She was then referred to our institution for consideration for surgery. At our institution, she had a liver MRI with hepatobiliary-specific contrast agent, gadoxetic acid, which identified nine focal liver lesions, involving all segments of the liver except the caudate. All lesions demonstrated T2 hyperintensity and no obvious diffusion restriction in any of the lesions (Figure 1). All lesions were hypointense relative to background liver on 10- and 20-min delayed phase imaging. The patient then proceeded to have a liver MRI with extracellular contrast agent, gadobutrol. All lesions demonstrated delayed retention of contrast on 10-min delayed phase imaging (Figure 2). Based on the two MRI’s, all lesions were thought to represent hemangiomas (some with atypical enhancement).
After obtaining informed consent, we performed an MRI of the liver with gadofosveset, an intravascular contrast agent, as part of an ongoing, prospective imaging study approved by the institutional research ethics board. Imaging was performed on a 3.0-Tesla (Philips Achieva™) magnet with an eight-channel body phased array coil covering the entire liver. The patient received a 10-mL intravenous dose of gadofosveset at 0.25 mmol/mL. Three-dimensional, fat-suppressed, spoiled gradient-echo axial T1-weighted (TE: 1.4 ms, TR: 3.0 ms, flip angle 10 degrees) contrast-enhanced imaging with short breath holds was performed. Images were acquired in the precontrast, arterial, portovenous, 2-, 5-, and 10-min delayed phases.
On gadofosveset-enhanced MRI, one lesion, seen in segment 7, demonstrated washout of contrast at 10-min delayed phase. All other lesions continued to demonstrated delayed retention of contrast at 10-min delayed phase as previously seen on gadobutrol-enhanced MRI (Figure 3).
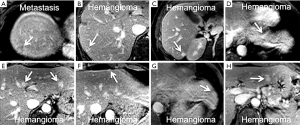
After discussion of the results with the patient, a decision to proceed with FOLFOX chemotherapy followed by a segment 7 liver resection. Pathology confirmed metastatic adenocarcinoma of the lesion in question. Follow-up imaging (>12 months) post-hepatectomy revealed that the other lesions remained stable, confirming benign etiology.
Discussion
This case demonstrates an example of a colorectal liver metastasis that demonstrates retention of contrast on MRI with an extracellular contrast agent, but washout of contrast on MRI with an intravascular contrast agent. Only four cases (from two studies) on the use of MRI with intravascular contrast agents to image colorectal liver metastases has been described in the literature, with similar findings (6,7). Two other studies have described the use of combined gadofosveset and gadoxetic acid, which suggest this may be helpful for improved detection of liver metastases (8,9). More experience is required to determine whether this phenomenon holds across multiple different lesions.
With extracellular contrast agents, late retention contrast in colorectal liver metastases is thought to be due to tumor fibrosis since extracellular contrast agents will leak into the fibrotic tissues via the extracellular space (8). It is thought that there would be minimal late retention of contrast into colorectal liver metastases with intravascular contrast agents since the contrast remains within the intravascular space (6,7).
Although intravascular contrast agents are rarely used for diagnosis of focal liver lesions with MRI, they are commonly used in the setting of contrast-enhanced ultrasound (5). Complete washout of contrast in metastases is used in contrast-enhanced ultrasound in order to distinguish benign from malignant lesions (5). Sustained enhancement in this setting virtually excludes hepatic metastases (5). However, contrast-enhanced ultrasound has significant limitations: it is operator-dependent and visualization of some lesions can be difficult. In addition, only one lesion can be imaged at any given time and evaluation of multiple lesions can be time consuming.
T2-weighted imaging was not helpful in this case as the colorectal liver metastasis demonstrated T2 hyperintensity that is indistinguishable from hemangiomas, possibly due to mucinous pathology. It is well-known that mucinous metastases can demonstrate T2-hyperintensity, mimicking benign hemangiomas (9).
Conclusions
This case report provides preliminary evidence to suggest that MRI with intravascular contrast agents, such as gadofosveset, may be a helpful clinical problem-solving tool in difficult-to-diagnose lesions in the preoperative patient with colorectal liver metastases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Cancer Facts & Figures 2017. American Cancer Society, 2017. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf
- Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, Alexander DD, Choti MA, Poston G. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol 2012;4:283-301. [PubMed]
- Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J. Factors influencing the natural history of colorectal liver metastases. Lancet 1994;343:1405-10. [Crossref] [PubMed]
- Doo KW, Lee CH, Choi JW, Lee J, Kim KA, Park CM. “Pseudo washout” sign in high-flow hepatic hemangioma on gadoxetic acid contrast-enhanced MRI mimicking hypervascular tumor. AJR Am J Roentgenol 2009;193:W490-6. [Crossref] [PubMed]
- Jang HJ, Yu H, Kim TK. Contrast-enhanced ultrasound in the detection and characterization of liver tumors. Cancer Imaging 2009;9:96-103. [PubMed]
- Milot L, Haider M, Foster L, McGregor C, Law C. Gadofosveset trisodium in the investigation of focal liver lesions in noncirrhotic liver: Early experience. J Magn Reson Imaging 2012;36:738-42. [Crossref] [PubMed]
- Cheung HM, Law C, Shoichet M, Karanicolas PJ, Coburn N, Milot L. Appearance of Focal Liver Lesions Using Contrast-Enhanced Magnetic Resonance Imaging Using Gadofosveset Trisodium, an Intravascular (Blood-Pool) Contrast Agent: A Pictorial Essay. Can Assoc Radiol J 2016;67:242-9. [Crossref] [PubMed]
- Maetani Y, Itoh K, Watanabe C, Shibata T, Ametani F, Yamabe H, Konishi J. MR imaging of intrahepatic cholangiocarcinoma with pathologic correlation. AJR Am J Roentgenol 2001;176:1499-507. [Crossref] [PubMed]
- Lacout A, El Hajjam M, Julie C, Lacombe P, Pelage JP. Liver metastasis of a mucinous colonic carcinoma mimicking a haemangioma in T2-weighted sequences. J Med Imaging Radiat Oncol 2008;52:580-2. [Crossref] [PubMed]


