Weight bearing cone beam CT scan versus gravity stress radiography for analysis of supination external rotation injuries of the ankle
Introduction
Ankle fractures that occur from excessive supination and external rotation (SER) are among the most common seen in orthopedic departments, and demand precise treatment because of potential biomechanical and clinical implications on the articulating weight-bearing surfaces of the ankle joint (1,2). Undisplaced or minimally displaced lateral malleolus fractures without medial injury are likely to be stable, and can be treated non-operatively with functional bracing and early mobilization (3-7). Lateral malleolar fractures with medial injury may be unstable, and are more frequently treated by operative reduction and internal fixation (8-10). Of all the methods that have been used to diagnose instability and investigate deltoid ligament integrity (clinical examination, weight-bearing radiographs, stress radiography, magnetic resonance imaging (MRI), arthroscopy, ultrasound), none have been shown to be cost-effective, rapid, reliable, and easy to use (8,10,11).
For fractures of uncertain stability, the current standard for determining the integrity of the medial side of the ankle is to obtain a gravity stress radiograph (8,12-17). Others have advocated for the use of weight-bearing radiographs, because gravity stress radiographs might overestimate the number of unstable ankle fractures (3-7,18). In these studies, weight-bearing radiographs have been shown to be predictive of stability, and patients with a normal mortise relationship can be successfully managed with immediate protected weight-bearing and functional treatment.
Generally, computed tomography (CT) scans are better than radiographs for visualization of bone detail, can generate 2D multiplanar images as well as 3D reconstructions, and can be very helpful for assessing fracture/dislocations in and around joints. A new portable dedicated extremity cone beam CT (CBCT) scanner (OnSight, Carestream Health, Rochester, NY, USA) has been approved by the Food and Drug Administration (FDA) for clinical use (19-21). We have recently gained experience using the CBCT scanner to obtain weight-bearing CT scans on SER ankle fractures of questionable stability and report our initial experience in this report. The primary aim of our study was to compare measures of medial clear space (MCS) on weight-bearing CBCT scans to MCS on gravity stress radiographs for determining the state of stability of ankle fractures classified as AO SER 44-B2 or Weber B (22,23). The secondary aim was to evaluate the details offered by multiplanar CBCT scans with respect to other findings that may be relevant to the care of patients with these types of injury. We hypothesized that MCS would be reduced on weight-bearing CBCT scan versus gravity stress radiographs and that the CT scans would provide other useful information regarding the configuration of the fracture.
Methods
Sample selection
Between April 2016 and February 2017, we screened patients presenting to our emergency department and clinical offices with an ankle injury. Patients underwent a standard history, physical examination, and routine plain radiographs to assess for injury. If X-rays revealed an isolated fibula fracture and there was clinical suspicion of medial injury and <5 mm of MCS widening on mortise view, the fracture was considered of uncertain stability and the patient was referred for gravity stress radiographs as the current standard of care. Patients were eligible for this cross-sectional study if they had an AO SER 44-B2, or Weber B, fracture confirmed by gravity stress radiograph and were 18 years or older. Patients were ineligible for the study if they were more than 7 days from the time of the gravity stress X-ray, were pregnant at the time of screening, had an open fracture, clinical signs of deformity, had a history of previous ankle surgery or trauma, had significant osteoarthritis or pre-existing ligamentous instability or pain in the affected ankle, were a prisoner, were non-English speaking, unable to provide informed consent, or could not bear weight on the involved extremity. Patients provided informed consent prior to participation in this study, which was approved by our institutional review board, conformed to the Helsinki Declaration and was compliant with HIPAA regulations.
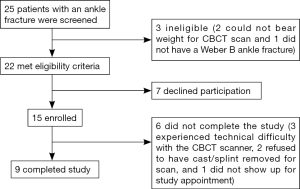
Twenty-five patients were screened, of which 22 met the study inclusion criteria and 15 patients enrolled (Figure 1). Two patients were ineligible because they could not bear weight for the CBCT scan and one patient did not have an AO SER 44-B2 fracture. Six patients did not complete the CT scan due to technical issues, leaving a total of 9 patients that completed the study. The mean patient age was 50.3 years (range: 33–61 years) and of the 9 patients, 6 were male [mean age: 48.2 years (33–57 years)] and 3 female [mean age: 54.7 years (45–61 years)].
Study procedure
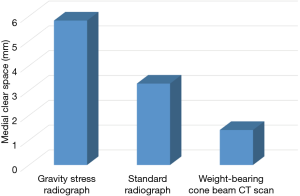
Each patient underwent a gravity stress radiograph as standard of care, and within 7 days also had a weight-bearing CBCT scan. To obtain the gravity stress radiograph, the patient’s leg was suspended over a semi-rigid lateral bolster placed above the level of the known fibula fracture. The X-ray tube was positioned to obtain a mortise view by angling the source 10 to 15 degrees in external rotation from the true antero-posterior plane (60 kVp and 3 mAs). The width of the MCS was measured as defined by the distance between the lateral border of the medial malleolus and the medial border of the talus at the level of the talar dome (8). The weight-bearing CBCT scan was obtained by having the patient stand on the custom foot plate of the scanner, resting the opposite leg with a bent knee on the top of the CT ring housing. The patient was instructed to bear full weight on the involved extremity, but was allowed to use the two arm handles of the device for balance and support during the CT scan (2 mm slices, 90 kVp and 5 mAs). The width of the MCS on CBCT image was measured as described above on the mid coronal CT slice for each patient. The readings were performed by a board certified orthopedic surgeon, fellowship trained in sports medicine, and with 25 years of experience in general orthopedics. Figure 2 shows MCS by imaging modality. The choice for or against operative management in each case was made by evaluating the gravity stress radiograph, patient specific factors, and surgeon preference without influence from the weight bearing CT scan. Five patients underwent operative open reduction and internal fixation while four were treated non-operatively with cast immobilization.

Statistical analysis
Descriptive statistics were calculated for age and sex. Wilcoxon signed-rank tests were used to compare MCS (mm) between the routine plain radiographs, the standard gravity stress radiographs, and weight-bearing CBCT scans. Means ± standard deviation are reported and the level of statistical significance was P<0.05. SAS 9.4 (SAS Institute, Cary, NC, USA) was used for statistical analysis.
Results
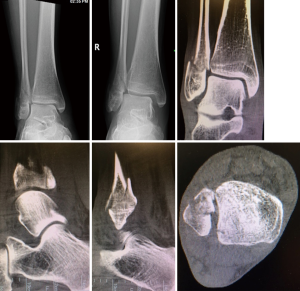
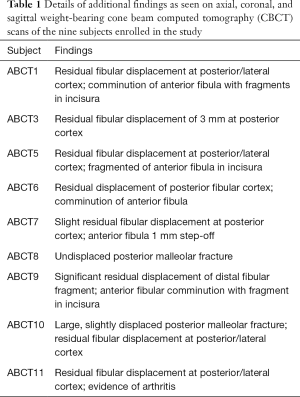
MCS measured on weight-bearing CBCT scan (1.41±0.41 mm) was less versus gravity stress radiographs (5.82±1.93 mm, P=0.004) and standard radiographs (3.28±1.63 mm, P=0.02). There was no statistically significant difference in MCS measured on standard radiographs versus gravity stress radiographs (P=0.11). Figure 3 shows MCS by imaging modality. Figure 4 and Table 1 show that there were no ankles that could be considered perfectly reduced by weight-bearing, all having one or more elements of displacement on review of all three planes on CBCT scan. Typical findings included posterior malleolar fracture, residual posterior and lateral displacement of the distal fibular fragment, as well as fibular comminution and joint asymmetry at the distal tibial incisura.
Full table
Discussion
We found that MCS measures on weight-bearing CBCT scans are less than those obtained on gravity stress X-rays (1.4 vs. 5.8 mm) in patients with AO 44-B2 ankle fractures. Similar to weight-bearing radiography, weight-bearing CBCT can predict stability of these ankle fractures by showing restoration of the MCS, and might be used to indicate patients for non-operative treatment. A SER mechanism of injury to the ankle frequently results in a lateral malleolus fracture as well as injury to the medial malleolus or deltoid ligament. When medial injury is significant, the ankle mortise may be unstable and the talus may shift laterally, resulting in significant changes in joint contact biomechanics (1,2,24,25). Unless the talus is anatomically restored to its position under the distal tibia and in the ankle mortise, it may represent a significant risk of the development of ankle arthritis and its associated symptoms. Recognition of instability, therefore, is the most important consideration when deciding on non-operative versus operative treatment of these types of injury, but can sometimes be difficult and controversial. This is especially true of the 44-B2 fracture as classified by the AO/OTA fracture and dislocation classification system (22). One of the currently accepted standard methods of determining medial injury and potential instability is the gravity stress radiograph as described by Michelson et al. (8,11-16). A standard mortise view is obtained and a positive finding is a MCS measurement of >4 or >1 mm more than the superior clear space. Gravity stress radiographs are well tolerated by patients, but some controversy remains in regards to their reproducibility, the definition of instability (4 or 5 mm of MCS widening or 1 mm more MCS widening than superior clear space) and whether or not stress overestimates the degree of instability of the ankle (12,15,16,26).
Another currently accepted method is a weight-bearing radiograph, which has been shown to be easy, pain free, safe and reliable, with excellent clinical outcome when patients were selected for non-operative treatment by this method (4-7,18,27). Hoshino et al. reported a series of 36 patients who had a lateral malleolus fracture, clinical findings of medial injury, and positive findings on stress radiographs. With evaluation by weight-bearing radiographs, only three patients had MCS widening and the remainder were successfully treated non-operatively (4). Two case series have shown that when stability can be illustrated on weight-bearing radiographs, non-operative treatment can be expected to deliver good clinical outcomes (5,6). These studies provide evidence to support non-operative treatment as a cost containment strategy and to avoid the morbidity and complications known to be associated with operative management of these fractures. In our series, based on the gravity stress radiograph, 5 of 9 subjects underwent surgery. If the clinical management decision was based on the weight bearing measure of MCS on CT scan, none of our 9 subjects would have had surgery.
Although other features of this injury pattern such as fibular shortening, fibular rotation, and comminution can sometimes be seen on plain radiographs, the nature of 2D images and overlapping of anatomical structures can make interpretation of X-rays difficult. CT scans are known to provide better bone detail and allow image viewing in multiple 2D planes. The images can also be post-processed to render 3D images that can be manipulated on a picture archiving communications station (PACS). A new dedicated extremity CBCT scanner has been approved by the FDA for market, and provides the unique ability to image subjects while weight-bearing.
While the weight-bearing CBCT scans revealed restoration of the MCS, many of the other CT images in our patients showed posterior malleolar involvement, residual fibular shortening, fibular rotation, fracture comminution, and asymmetry of the distal tibiofibular joint. With regard to our secondary aim, there were no ankles that could be considered perfectly reduced by weight-bearing, all having one or more of the above elements of displacement on review of all three planes on CBCT scan. The implications of these additional findings on fracture care and on patient outcomes is currently unknown, but many patients have continued symptoms even when X-rays show an adequate anatomic restoration of the ankle mortise. Further clinical research is necessary to determine if any of these CBCT findings are related to patient outcomes.
Potential limitations of our study are the small sample size, and the fact that the sample represents only 9 of a potential 25 eligible subjects. Because our patients were allowed to rest the healthy leg on the CT ring housing, and were allowed to use the two arm handles of the device for balance and support during the CT scan, true full weight bearing may not have been achieved. Other studies have demonstrated approximately 5–10% rate of instability demonstrated on weight-bearing radiographs, so it is estimated that it would take 10 to 20 patients to find 1 unstable fracture on weight-bearing CBCT scan (4,5). We recognize that by the nature of our study requiring our patients to bear weight on a fractured ankle, we may have selected the most stable of the ankles, which simply confirmed stability with the weight-bearing CBCT and limits the generalizability of the study results.
The findings of this study suggest that similar to weight-bearing radiography, weight-bearing CBCT scan can predict stability of AO 44-B2, or Weber B, ankle fractures by showing restoration of the MCS. The detailed findings of CBCT scan, however, reveal persistent fracture displacement and non-anatomic restoration of the ankle syndesmosis with uncertain implications on the biomechanics of the ankle joint and on the clinical outcome of non-operative treatment for this injury.
Acknowledgements
This study was funded by Carestream Health, Inc. and has not been published elsewhere.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am 1976;58:356-7. [Crossref] [PubMed]
- Harris J, Fallat L. Effects of isolated Weber B fibular fractures on the tibiotalar contact area. J Foot Ankle Surg 2004;43:3-9. [Crossref] [PubMed]
- Stewart C, Saleem O, Mukherjee DP, Suk M, Marymont J, Anissian L. Axial load weightbearing radiography in determining lateral malleolus fracture stability: a cadaveric study. Foot Ankle Int 2012;33:548-52. [Crossref] [PubMed]
- Hoshino CM, Nomoto EK, Norheim EP, Harris TG. Correlation of weightbearing radiographs and stability of stress positive ankle fractures. Foot Ankle Int 2012;33:92-8. [Crossref] [PubMed]
- Holmes JR, Acker WB 2nd, Murphy JM, McKinney A, Kadakia AR, Irwin TA. A Novel Algorithm for Isolated Weber B Ankle Fractures: A Retrospective Review of 51 Nonsurgically Treated Patients. J Am Acad Orthop Surg 2016;24:645-52. [Crossref] [PubMed]
- Hastie GR, Akhtar S, Butt U, Baumann A, Barrie JL. Weightbearing Radiographs Facilitate Functional Treatment of Ankle Fractures of Uncertain Stability. J Foot Ankle Surg 2015;54:1042-6. [Crossref] [PubMed]
- Weber M, Burmeister H, Flueckiger G, Krause FG. The use of weightbearing radiographs to assess the stability of supination-external rotation fractures of the ankle. Arch Orthop Trauma Surg 2010;130:693-8. [Crossref] [PubMed]
- Egol KA, Amirtharajah M, Tejwani NC, Capla EL, Koval KJ. Ankle stress test for predicting the need for surgical fixation of isolated fibular fractures. J Bone Joint Surg Am 2004;86-A:2393-8. [Crossref] [PubMed]
- Yablon IG, Wasilewski S. Isolated fracture of the lateral malleolus. Orthopedics 1981;4:301-4. [PubMed]
- Stufkens SA, van den Bekerom MP, Knupp M, Hintermann B, van Dijk CN. The diagnosis and treatment of deltoid ligament lesions in supination–external rotation ankle fractures: a review. Strategies Trauma Limb Reconstr 2012;7:73-85. [Crossref] [PubMed]
- van den Bekerom MP, Mutsaerts EL, van Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg 2009;129:227-35. [Crossref] [PubMed]
- Gill JB, Risko T, Raducan V, Grimes JS, Schutt RC Jr. Comparison of manual and gravity stress radiographs for the evaluation of supination-external rotation fibular fractures. J Bone Joint Surg Am 2007;89:994-9. [PubMed]
- Michelson JD, Varner KE, Checcone M. Diagnosing deltoid injury in ankle fractures: the gravity stress view. Clin Orthop Relat Res 2001.178-82. [Crossref] [PubMed]
- McConnell T, Creevy W, Tornetta P 3rd. Stress examination of supination external rotation-type fibular fractures. J Bone Joint Surg Am 2004;86-A:2171-8. [Crossref] [PubMed]
- Park SS, Kubiak EN, Egol KA, Kummer F, Koval KJ. Stress radiographs after ankle fracture: the effect of ankle position and deltoid ligament status on medial clear space measurements. J Orthop Trauma 2006;20:11-8. [Crossref] [PubMed]
- Schock HJ, Pinzur M, Manion L, Stover M. The use of gravity or manual-stress radiographs in the assessment of supination-external rotation fractures of the ankle. J Bone Joint Surg Br 2007;89:1055-9. [Crossref] [PubMed]
- den Bekerom MP, Mutsaerts EL, Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: A systematic review of the literature. Arch Orthop Trauma Surg 2009;129:227-35. [Crossref] [PubMed]
- Seidel A, Krause F, Weber M. Weightbearing vs Gravity Stress Radiographs for Stability Evaluation of Supination-External Rotation Fractures of the Ankle. Foot Ankle Int 2017;38:736-44. [Crossref] [PubMed]
- Carrino JA, Al Muhit A, Zbijewski W, Thawait GK, Stayman JW, Packard N, Senn R, Yang D, Foos DH, Yorkston J, Siewerdsen JH. Dedicated cone-beam CT system for extremity imaging. Radiology 2014;270:816-24. [Crossref] [PubMed]
- Tuominen EK, Kankare J, Koskinen SK, Mattila KT. Weight-bearing CT imaging of the lower extremity. AJR Am J Roentgenol 2013;200:146-8. [Crossref] [PubMed]
- Zbijewski W, De Jean P, Prakash P. A cone-beam CT system for musculoskeletal extremities with advanced multi-mode imaging capabilities. Int J Comput Assist Radiol Surg 2011;6:S19-21.
- Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007;21:S1-133. [Crossref] [PubMed]
- Weber BG. Die Verletzungen des oberen Sprunggelenkes. Bern, Switzerland: Huber Verlag, 1972.
- Moody ML, Koeneman J, Hettinger E, Karpman RR. The effects of fibular and talar displacement on joint contact areas about the ankle. Orthop Rev 1992;21:741-4. [PubMed]
- Lloyd J, Elsayed S, Hariharan K, Tanaka H. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int 2006;27:793-6. [Crossref] [PubMed]
- Murphy JM, Kadakia AR, Irwin TA. Variability in radiographic medial clear space measurement of the normal weight-bearing ankle. Foot Ankle Int 2012;33:956-63. [Crossref] [PubMed]
- Michelson JD, Magid D, McHale K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma 2007;21:307-15. [Crossref] [PubMed]