Assessment of myocardial oxygenation with MRI
As an aerobic organ in a living body, the beating heart relies almost exclusively on the oxidation of energy-providing substrates such as free fatty acids (60-90%) for its primary contractile function. Specifically, chemical energy is generally produced in aerobic metabolic pathways through oxidative phosphorylation of ADP to ATP. Myocytes utilize the chemical energy stored in ATP molecules and transform it into mechanical energy. Accordingly, cardiac cells have to consume large amounts of O2 for the contraction process, which accounts for over 80% of oxygen cost. The remaining <20% is consumed by other physiological processes not directly associated with contraction, i.e., membrane depolarization and repolarization. For this reason, the heart can only develop a small oxygen debt. Oxygen supply and demand has to match to maintain normal myocardial contractility.
Myocardial ischemia exists when the supply of oxygen to the myocardial tissue is inadequate for the metabolic oxygen demand of myocardium. This is usually caused by upstream coronary artery stenosis that reduces blood supply (coronary artery disease or CAD). Clinically, myocardial hypoxemia results in arrhythmia, angina, and regional or global impairment of ventricular function (1). Severe and prolonged imbalance between oxygen supply and demand will eventually lead to myocardial infarction. In addition, ischemia may still present even though the coronary artery flow is maintained due to an imbalance between oxygen supply and demand secondary to the increased myocardial metabolic requirements. As with severe systemic hypertension, the whole heart becomes ischemic. Measuring and quantifying the balance of myocardial oxygenation would provide direct assessment of the status of myocardial oxidative metabolism and ischemic status.
In current clinical practice, X-ray angiography is considered the gold standard for diagnosis of coronary artery stenosis. However, measurement of coronary artery stenosis by angiography is not always a reliable indication of the functional consequence of stenosis in CAD patients. Any variations, e.g., irregular atherosclerotic plaque, variable collateral flow, preexisting ventricle remodeling, etc. will alter the effect of coronary artery stenosis. Currently, cardiac PET has been the major image modality for absolute quantification of regional myocardial perfusion and oxygen metabolism (2). Investigators have shown that PET permits accurate quantification of regional myocardial blood flow (MBF) (3-5) with 15O-water, and of myocardial oxygen consumption rate (MVO2) (6-9) with 11carbon-acetate. Perfusion-MVO2 (supply-demand) mismatches were found in CAD patients with significant single-vessel left anterior descending (LAD) stenosis (>70%) using 11C-acetate PET, despite normal regional left ventricular contractile function at rest (10). Of note, quantitative measurements of MVO2 and oxygen extraction fraction (OEF) using 15O2-labeled oxygen gas were also reported in animals and healthy volunteers (11), and evaluated in patients (12). However, low spatial resolution (not suitable for the detection of subendocardial perfusion defects), relatively long acquisition time, limited availability, relative high cost, and ionizing radiation discourage the widespread use of PET for these purposes.
MRI is a non-invasive imaging modality that provides excellent image spatial resolution and soft tissue contrast, does not require iodinated contrast media or ionizing radiation, and is widely available. Cardiac functional MRI demonstrated myocardial blood oxygenation qualitatively evaluated in animals and humans using the BOLD (Blood Oxygen Level Dependence) effect (13-19), which is the fundamental mechanism for detecting tissue and blood oxygenation in MRI (20-23). Thulborn et al. (24) first recognized the BOLD effect: that the presence of paramagnetic deoxyhemoglobin in red blood cell affects blood T2 relaxation rate in vitro. This observation was confirmed and validated by others (25-30). Early studies in the heart indicated myocardial relaxation time T2* (1/T2* = 1/T2 + 1/T2' and T2' is related to the magnetic field inhomogeneity) changes with alterations in total tissue deoxyhemoglobin concentration. Since then, myocardial T2* or T2*-weighted imaging, which is usually acquired by gradient-echo (GE) sequences, has been explored by many investigators to assess the change in myocardial oxygenation in cardiac MRI (31-35).
Semi-quantitative assessment of myocardial oxygenation
In earlier work, T2* contrast was usually applied to assess the change in myocardial oxygenation following pharmaceutically induced hyperemia (Table 1) (36,37). The typical sequence was a segmented multi-echo gradient echo with ECG triggering and black-blood dual-inversion-pulse preparation. Data acquisition occurred mid-diastole to minimize cardiac motion. Because of the T1 effects from heart rate variation, e.g., from resting to vasodilation, absolute T2* value is preferred for assessing BOLD contrast. From literature published so far, the sensitivity and specificity to detect significant coronary artery stenosis are approximately 90% and 70%, respectively.
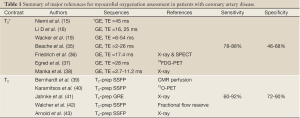
Full Table
However, T2* contrast is sensitive to bulk susceptibility artifacts (19), field inhomogeneity, and magnetic field shimming status (28). Reproducibility of T2* measurement is poor for different regions of the myocardium on an intra- and inter-subject basis. In contrast, T2 or T2-weighted contrasts are more physiologically relevant. Compared to T2* contrast, sensitivity to oxygenation with T2 contrast is reduced for all vessel sizes, but it is much less sensitive to changes in hematocrit, temperature, and field inhomogeneity. In the heart, capillaries contribute over 90% of the microvascular blood volume (44,45). The change in T2 due to changes in deoxyhemoglobin content reaches its maximum in capillary-size vessels (46).
Because T2 contrast is most sensitive to the changes in susceptibility and diffusion in the capillary system, T2 may be a useful candidate for imaging microvasculature and vasodilatory alternations in myocardium quantitatively. Foltz and et al. (47) have demonstrated a significant correlation between regional myocardial T2 in the left anterior descending (LAD) coronary artery territory and oxygen content in the LAD coronary vein. Ghugre et al. (48) applied T2 BOLD contrast to image infarction and remote regions using an acute myocardial infarction porcine model. The changes of myocardial T2 in both regions were observed throughout the infarction healing, which may indicate the status of left ventricle remodeling. In comparison with the T2* method, T2 contrast clearly benefits from much higher image quality with acceptable BOLD sensitivity (approximately 10% at 1.5 T, and 15% at 3 T). Another interesting method is to use phase resolved BOLD MRI (49) that can readily assess changes in myocardial oxygenation and blood volume in different cardiac cycles. Myocardial ischemia can be detected even at rest with this approach (50).
Recent clinical applications of T2-based method has primarily used T2-weighted imaging that was first proposed by Li et al. (51) and then validated in a canine model (52). Advanced development in cardiac TrueFISP (True Fast Imaging with Steady State precession) imaging allows high quality of T2-weighted TrueFISP to assess BOLD contrast in a clinical setting (39,40,43). The typical sequence is a 2-dimensional T2-prepared segmented TrueFISP acquisition with a T2 preparation time of 40 ms. For the minimization of cardiac and respiratory motion, data is acquired mid-diastole with breath-hold by the subject. BOLD contrast has to be determined before and after adenosine administration from the change in signal intensity. Figure 1 shows the detection of coronary artery stenosis using a BOLD index derived from T2-weighted images, demonstrating the sensitivity of this technique. Several manuscripts have been recently published using this technique. Relatively high sensitivity and specificity can be achieved >90% in the detection of coronary artery diseases in comparison with PET perfusion (53), X-ray angiography (38,41), and fractional flow reserve (42). Interestingly, by comparison with PET or MRI perfusion measurements, regions of deoxygenation sometimes mismatch with the regions of hypoperfusion (43,53), and tissue oxygenation correlates poorly with quantitative coronary angiography (43). The underlying mechanism remains unclear, but it postulated that myocardial autoregulation, ATP usage, and myocardial blood volume may play certain roles for this process.

Quantitative assessment of myocardial oxygenation
Quantitative myocardial oximetry was developed previously by establish the relationship between blood T2 and oxygen saturation (30). The method was further evaluated in vivo for coronary sinus oxygenation in adults (54) and in infants (55). Using the same approach, measurements of global left ventricular MVO2 and whole body oxygen consumption (VO2) were reported by Yang et al. (56). Both data are very comparable with reported PET and other invasive methods (MVO2: 11±3 vs. 10±3 mL/min per 100 g LV mass; VO2: 3.8±0.8 vs. 3.5 mL/min/kg body weight). Furthermore, the reproducibility of their measurements is relatively high (coefficient of repeatability of 1.0 mL/min per 100 g LV mass).
Another approach to assess myocardial oxygenation is to measure myocardial oxygenation response during a vasodilation or stress (hyperemia). A MRI method was developed to derive hyperemic myocardial OEF by taking advantage of the BOLD effect in myocardial T2 (57). When myocardial flow increases during hyperemia, normal myocardial T2 will increase secondary to reduced deoxyhemoglobin concentration. With excessive oxygen supply, myocardial OEF will reduce in normal myocardial tissue, but will remain the same or even increase in ischemic tissue. A two-compartment diffusion model was created to calculate hyperemic OEF, based on known or assumed resting myocardial OEF. The data acquisition is performed using a 2D multi-contrast segmented turbo spin-echo sequence to generate T2-weighted images that are used to calculate pixel-by-pixel T2 maps.
In a validation study using a coronary artery disease model in canines, PET imaging was used as the reference method to measure myocardial transmural OEF and MVO2 (58). Overall there were no significant errors and the MRI OEF results were closely correlated with the reference PET measurements. MRI measurement of MVO2 slightly overestimated PET results, but with a very strong linear correlation (slope =0.83; intercept =1.41; r=0.86, P<0.001). These technical developments demonstrated promising alternatives to nuclear techniques because they could be used for serial assessments of myocardial oxygenation in settings of regional or global myocardial ischemia without worrying about excessive radiation.
In the latest development, another T2 sequence, bright-blood T2-prepared-gradient-echo or T2-prepared TrueFISP sequence, was modified to calculate myocardial T2 maps using 4-5 T2-weighted images within one breath-hold (59). Resting OEF in the coronary sinus, representing global myocardial OEF, can also be calculated through a blood-oxygen model. The main limitations of the sequence are relatively low spatial resolution and limited precision. The sequence is also sensitive to both respiratory and cardiac motion, particularly at higher heart rates. In addition, calculation of myocardial OEF remains complicated. Further technical improvement is needed to reduce motion artifacts, acquire more T2-weighted images to increase the precision of myocardial T2 measurements, and to streamline model calculation for clinical practices.
In summary, MRI based myocardial oxygenation imaging is an attractive non-invasive approach to assess myocardial oxygen supply and demand. Although the T2* method demonstrated great sensitivity detecting changes in myocardial oxygen content, T2-based high-contrast SSFP imaging has earned an important role in a clinical setting, owning to its good sensitivity and high image quality. Quantitative measures using either absolute myocardial T2 or related modeling for OEF calculation could allow consecutive monitoring of dose response of medical therapy. However, more technical innovations (multi-slice, higher spatial resolution for endocardial assessment, better sensitivity, etc) and systematic evaluation are warranted before exploring for full clinical applications.
Acknowledgements
The author thanks David Muccigrosso for assisting the edition of the manuscript.
Disclosure: The author declares no conflict of interest.
References
- Braunwald E. eds. Heart Disease. 6th Edition, Philadelphia: W.B. Saunders Company, 2001.
- Segall G. Assessment of myocardial viability by positron emission tomography. Nucl Med Commun 2002;23:323-30.
- Bergmann SR, Herrero P, Markham J, et al. Noninvasive quantitation of myocardial blood flow in human subjects with oxygen-15-labeled water and positron emission tomography. J Am Coll Cardiol 1989;14:639-52.
- Gropler RJ, Geltman EM, Sampathkumaran K, et al. Comparison of carbon-11-acetate with fluorine-18-fluorodeoxyglucose for delineating viable myocardium by positron emission tomography. J Am Coll Cardiol 1993;22:1587-97.
- Sun KT, Yeatman LA, Buxton DB, et al. Simultaneous measurement of myocardial oxygen consumption and blood flow using [1-carbon-11]acetate. J Nucl Med 1998;39:272-80.
- Brown MA, Myears DW, Bergmann SR. Validity of estimates of myocardial oxidative metabolism with carbon-11 acetate and positron emission tomography despite altered patterns of substrate utilization. J Nucl Med 1989;30:187-93.
- Buxton DB, Nienaber CA, Luxen A, et al. Noninvasive quantitation of regional myocardial oxygen consumption in vivo with [1-11C]acetate and dynamic positron emission tomography. Circulation 1989;79:134-42.
- Yamamoto Y, de Silva R, Rhodes CG, et al. Noninvasive quantification of regional myocardial metabolic rate of oxygen by 15O2 inhalation and positron emission tomography. Experimental validation. Circulation 1996;94:808-16.
- Gropler RJ, Geltman EM, Sampathkumaran K, et al. Functional recovery after coronary revascularization for chronic coronary artery disease is dependent on maintenance of oxidative metabolism. J Am Coll Cardiol 1992;20:569-77.
- Janier MF, André-Fouet X, Landais P, et al. Perfusion-MVO2 mismatch during inotropic stress in CAD patients with normal contractile function. Am J Physiol 1996;271:H59-67.
- Iida H, Rhodes CG, Araujo LI, et al. Noninvasive quantification of regional myocardial metabolic rate for oxygen by use of 15O2 inhalation and positron emission tomography. Theory, error analysis, and application in humans. Circulation 1996;94:792-807.
- Agostini D, Iida H, Takahashi A, et al. Regional myocardial metabolic rate of oxygen measured by O2-15 inhalation and positron emission tomography in patients with cardiomyopathy. Clin Nucl Med 2001;26:41-9.
- Atalay MK, Forder JR, Chacko VP, et al. Oxygenation in the rabbit myocardium: assessment with susceptibility-dependent MR imaging. Radiology 1993;189:759-64.
- Balaban RS, Taylor JF, Turner R. Effect of cardiac flow on gradient recalled echo images of the canine heart. NMR Biomed 1994;7:89-95.
- Niemi P, Poncelet BP, Kwong KK, et al. Myocardial intensity changes associated with flow stimulation in blood oxygenation sensitive magnetic resonance imaging. Magn Reson Med 1996;36:78-82.
- Li D, Dhawale P, Rubin PJ, et al. Myocardial signal response to dipyridamole and dobutamine: demonstration of the BOLD effect using a double-echo gradient-echo sequence. Magn Reson Med 1996;36:16-20.
- Reeder SB, Holmes AA, McVeigh ER, et al. Simultaneous noninvasive determination of regional myocardial perfusion and oxygen content in rabbits: toward direct measurement of myocardial oxygen consumption at MR imaging. Radiology 1999;212:739-47.
- Atalay MK, Reeder SB, Zerhouni EA, et al. Blood oxygenation dependence of T1 and T2 in the isolated, perfused rabbit heart at 4.7T. Magn Reson Med 1995;34:623-7.
- Wacker CM, Bock M, Hartlep AW, et al. Changes in myocardial oxygenation and perfusion under pharmacological stress with dipyridamole: assessment using T*2 and T1 measurements. Magn Reson Med 1999;41:686-95.
- Belliveau JW, Kennedy DN Jr, McKinstry RC, et al. Functional mapping of the human visual cortex by magnetic resonance imaging. Science 1991;254:716-9.
- Kwong KK, Belliveau JW, Chesler DA, et al. Dynamic magnetic resonance imaging of human brain activity during primary sensory stimulation. Proc Natl Acad Sci U S A 1992;89:5675-9.
- Ogawa S, Menon RS, Tank DW, et al. Functional brain mapping by blood oxygenation level-dependent contrast magnetic resonance imaging. A comparison of signal characteristics with a biophysical model. Biophys J 1993;64:803-12.
- Ogawa S, Lee TM, Nayak AS, et al. Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields. Magn Reson Med 1990;14:68-78.
- Thulborn KR, Waterton JC, Matthews PM, et al. Oxygenation dependence of the transverse relaxation time of water protons in whole blood at high field. Biochim Biophys Acta 1982;714:265-70.
- Gomori JM, Grossman RI, Yu-Ip C, et al. NMR relaxation times of blood: dependence on field strength, oxidation state, and cell integrity. J Comput Assist Tomogr 1987;11:684-90.
- Wright GA, Hu BS, Macovski A. 1991 I.I. Rabi Award. Estimating oxygen saturation of blood in vivo with MR imaging at 1.5 T. J Magn Reson Imaging 1991;1:275-83.
- Hoppel BE, Weisskoff RM, Thulborn KR, et al. Measurement of regional blood oxygenation and cerebral hemodynamics. Magn Reson Med 1993;30:715-23.
- Graham GD, Zhong J, Petroff OA, et al. BOLD MRI monitoring of changes in cerebral perfusion induced by acetazolamide and hypercarbia in the rat. Magn Reson Med 1994;31:557-60.
- Barth M, Moser E. Proton NMR relaxation times of human blood samples at 1.5 T and implications for functional MRI. Cell Mol Biol (Noisy-le-grand) 1997;43:783-91.
- Li KC, Wright GA, Pelc LR, et al. Oxygen saturation of blood in the superior mesenteric vein: in vivo verification of MR imaging measurements in a canine model. Work in progress. Radiology 1995;194:321-5.
- Li D, Oellerich WF, Beck G, et al. Assessment of myocardial response to pharmacologic interventions using an improved MR imaging technique to estimate T2 values. AJR Am J Roentgenol 1999;172:141-5.
- Li D, Wang Y, Waight DJ. Blood oxygen saturation assessment in vivo using T2* estimation. Magn Reson Med 1998;39:685-90.
- Li D, Waight DJ, Wang Y. In vivo correlation between blood T2* and oxygen saturation. J Magn Reson Imaging 1998;8:1236-9.
- Wacker CM, Bock M, Hartlep AW, et al. BOLD-MRI in ten patients with coronary artery disease: evidence for imaging of capillary recruitment in myocardium supplied by the stenotic artery. MAGMA 1999;8:48-54.
- Beache GM, Herzka DA, Boxerman JL, et al. Attenuated myocardial vasodilator response in patients with hypertensive hypertrophy revealed by oxygenation-dependent magnetic resonance imaging. Circulation 2001;104:1214-7.
- Friedrich MG, Niendorf T, Schulz-Menger J, et al. Blood oxygen level-dependent magnetic resonance imaging in patients with stress-induced angina. Circulation 2003;108:2219-23.
- Egred M, Waiter GD, Semple SI, et al. Blood oxygen level-dependent (BOLD) magnetic resonance imaging in patients with dypiridamole induced ischaemia; a PET comparative study. Int J Cardiol 2007;115:36-41.
- Manka R, Paetsch I, Schnackenburg B, et al. BOLD cardiovascular magnetic resonance at 3.0 tesla in myocardial ischemia. J Cardiovasc Magn Reson 2010;12:54.
- Bernhardt P, Manzke R, Bornstedt A, et al. Blood oxygen level-dependent magnetic resonance imaging using T2-prepared steady-state free-precession imaging in comparison to contrast-enhanced myocardial perfusion imaging. Int J Cardiol 2011;147:416-9.
- Karamitsos TD, Arnold JR, Pegg TJ, et al. Patients with syndrome X have normal transmural myocardial perfusion and oxygenation: a 3-T cardiovascular magnetic resonance imaging study. Circ Cardiovasc Imaging 2012;5:194-200.
- Jahnke C, Gebker R, Manka R, et al. Navigator-gated 3D blood oxygen level-dependent CMR at 3.0-T for detection of stress-induced myocardial ischemic reactions. JACC Cardiovasc Imaging 2010;3:375-84.
- Walcher T, Manzke R, Hombach V, et al. Myocardial perfusion reserve assessed by T2-prepared steady-state free precession blood oxygen level-dependent magnetic resonance imaging in comparison to fractional flow reserve. Circ Cardiovasc Imaging 2012;5:580-6.
- Arnold JR, Karamitsos TD, Bhamra-Ariza P, et al. Myocardial oxygenation in coronary artery disease: insights from blood oxygen level-dependent magnetic resonance imaging at 3 tesla. J Am Coll Cardiol 2012;59:1954-64.
- Bauer WR, Nadler W, Bock M, et al. Theory of the BOLD effect in the capillary region: an analytical approach for the determination of T2 in the capillary network of myocardium. Magn Reson Med 1999;41:51-62.
- Kaul S, Jayaweera AR. Coronary and myocardial blood volumes: noninvasive tools to assess the coronary microcirculation? Circulation 1997;96:719-24.
- Boxerman JL, Hamberg LM, Rosen BR, et al. MR contrast due to intravascular magnetic susceptibility perturbations. Magn Reson Med 1995;34:555-66.
- Foltz WD, Huang H, Fort S, et al. Vasodilator response assessment in porcine myocardium with magnetic resonance relaxometry. Circulation 2002;106:2714-9.
- Ghugre NR, Ramanan V, Pop M, et al. Myocardial BOLD imaging at 3 T using quantitative T2: application in a myocardial infarct model. Magn Reson Med 2011;66:1739-47.
- Zhou X, Tsaftaris SA, Liu Y, et al. Artifact-reduced two-dimensional cine steady state free precession for myocardial blood- oxygen-level-dependent imaging. J Magn Reson Imaging 2010;31:863-71.
- Tsaftaris SA, Zhou X, Tang R, et al. Detecting Myocardial Ischemia at Rest with Cardiac Phase-Resolved BOLD CMR. Circ Cardiovasc Imaging 2013;6:311-9.
- Wright KB, Klocke FJ, Deshpande VS, et al. Assessment of regional differences in myocardial blood flow using T2-weighted 3D BOLD imaging. Magn Reson Med 2001;46:573-8.
- Fieno DS, Shea SM, Li Y, et al. Myocardial perfusion imaging based on the blood oxygen level-dependent effect using T2-prepared steady-state free-precession magnetic resonance imaging. Circulation 2004;110:1284-90.
- Karamitsos TD, Leccisotti L, Arnold JR, et al. Relationship between regional myocardial oxygenation and perfusion in patients with coronary artery disease: insights from cardiovascular magnetic resonance and positron emission tomography. Circ Cardiovasc Imaging 2010;3:32-40.
- Foltz WD, Merchant N, Downar E, et al. Coronary venous oximetry using MRI. Magn Reson Med 1999;42:837-48.
- Nield LE, Qi X, Yoo SJ, et al. MRI-based blood oxygen saturation measurements in infants and children with congenital heart disease. Pediatr Radiol 2002;32:518-22.
- Yang Y, Foltz WD, Merchant N, et al. Noninvasive quantitative measurement of myocardial and whole-body oxygen consumption using MRI: initial results. Magn Reson Imaging 2009;27:147-54.
- Zheng J, Wang J, Nolte M, et al. Dynamic estimation of the myocardial oxygen extraction ratio during dipyridamole stress by MRI: a preliminary study in canines. Magn Reson Med 2004;51:718-26.
- McCommis KS, Goldstein TA, Abendschein DR, et al. Quantification of regional myocardial oxygenation by magnetic resonance imaging: validation with positron emission tomography. Circ Cardiovasc Imaging 2010;3:41-6.
- McCommis KS, O’Connor R, Lesniak D, et al. Quantification of global myocardial oxygenation in humans: initial experience. J Cardiovasc Magn Reson 2010;12:34.


