Imaging of shoulder instability
Introduction
Shoulder dislocations account for 90% of shoulder instability cases and usually occur after a fall during sport or work activities (1). This glenohumeral joint instability has been defined with the acronyms TUBS (traumatic, unidirectional, Bankart, surgery is the main treatment) (2). Associated injuries to the labrum, to the glenoid bone, described in up to 40% of the cases (3), and to the humeral head (known as Hill-Sachs lesions), have been described in 38–88% of the cases (4,5). They may influence prognosis and treatment. Imaging methods play a paramount role in identifying and quantifying theses injuries and posing differential diagnosis with another cause of instability. These causes include AMBRII (atraumatic, multidirectional, bilateral, rehabilitation is the main treatment, inferior capsular tightening and interval reconstruction in case patients need surgery) (6), and a group of subtle conditions defined as “minor shoulder instability”, that are also responsible for shoulder pain and dysfunction (7). Two entities are included under this concept, AIOS (acquired instability, overstressed shoulder) and AMSI (atraumatic minor shoulder instability) (8,9).
This extended review aims to pinpoint the usefulness of imaging methods in diagnosing and quantifying shoulder injuries secondary to instability. These findings may influence prognosis and treatment.
Radiography
In spite of the wide use of ultrasonography and magnetic resonance imaging (MRI) as first line of investigation for shoulder pain, radiography remains as an essential tool that provide a general overview of the shoulder anatomy helping to rule-out unsuspected serious conditions, such as tumors or arthritis.
Once indicated, at least three views are recommended in the shoulder trauma protocol, two of which should be orthogonal (10) (Figure 1).
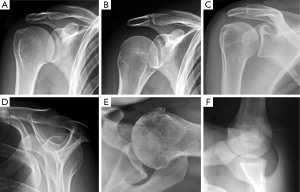
When shoulder dislocation is suspected, straight anteroposterior (AP) view (neutral or with internal/external arm rotation) can evaluate the shoulder for fracture or dislocation. In the AP view the observer will see the humeral head overlapping the glenoid obscuring the glenohumeral joint space, limiting its assessment. Therefore, it should be complemented with scapular Y view and/or glenoid profile view (Grashey view). Anterior dislocation is going to be apparent in the AP view, but posterior dislocation can be missed in non-experienced radiography readers. Axillary lateral view may be difficult to perform in these patients because of the pain and limited motion. It assesses the anterior rim of the glenoid.
When shoulder instability becomes recurrent, a complete radiographic study may help get to the diagnosis. Radiographs show osseous lesions of the humerus or glenoid in 95% of patients with chronic anterior instability. The glenoid profile view (West-Point or Bernageau) assesses the anteroinferior glenoid rim and showed an osseous lesion of the glenoid in 78.8% of the shoulders with recurrent dislocation (11). In this projection, we can identify the “cliff sign”, a large glenoid defect and the “blunted angle sign”, a rounding off of the anterior glenoid (12).
Anterior dislocations represent about 90–95% of all shoulder dislocations. In these cases, a compression fracture of the posterior and superior part of the humeral head (Hill-Sachs lesion) or blurring of the anterior border of the glenoid suggesting a bony Bankart lesion might be seen. Bone fragments may be seen rarely.
Posterior shoulder dislocations only account for 3–5% of dislocations, but they can be missed in about 50% of the cases (12). In posterior dislocation, AP films may resemble normal anatomical relationship, but the identification of the reverse Hill-Sachs lesion may be the clue of suspecting the presence of a posterior dislocation. This posterior dislocation of the humeral head can be accurately demonstrated by the scapular Y and axillary views (Figure 2).

Finally, shoulder may suffer of unusual dislocations. Luxatio erecta represents around 0.5–1% of shoulder dislocation and consists in an inferior shift of the humeral head that loses contact with the glenoid cavity (13). The arm appears held upward because of fixed abduction.
Multidetector computed tomography (MDCT)
CT is mainly indicated after traumatic injury of the shoulder to rule out fractures not visible in radiographs or to assess the extent and severity of fractures already depicted in previous radiographs. CT is also useful to assess humeral and glenoid version. Excessive version can lead to instability (Figure 3). Normal glenoid version has been reported close to 0°. Slight retroversion is more frequent than retroversion, with values generally lower than 10° in either direction (14).
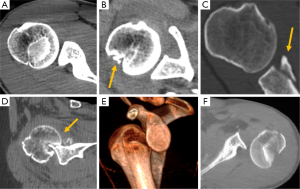
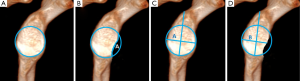
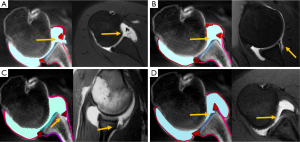
In shoulder dislocation assessment of Bankart fragment size is better performed by CT. Fragments involving more than 25% of the width of the antero-inferior glenoid may be an indication for open surgical repair and bone grafting. This percentage is equivalent to 6–8 mm of width loss, given that the average glenoid width at the level of the bare area is 24–26 mm (15,16). Due to bone loss, the bony glenoid may appear as an inverted pear-shaped structure with the inferior half of the glenoid having a shorter diameter than the superior half of the glenoid (17). The percentage of anterior glenoid defect can also be measure on a sagittal section of the most lateral portion of the glenoid (18). Accurate methods for quantifying glenoid bone loss are the best-fit circle surface area or “Pico method” and the Glenoid Width Index method, especially when using three-dimensional CT (3DCT) (19). Percentages of bone loss above 20% using the Pico Method are associated to recurrent dislocation (20). The % of bone loss can be estimated by drawing a circle over the intact posteroinferior margins of the injured glenoid or by measuring the contralateral glenoid (Figure 4).
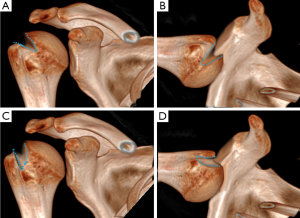
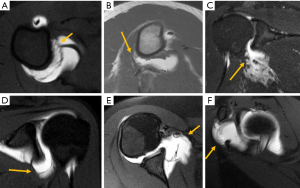
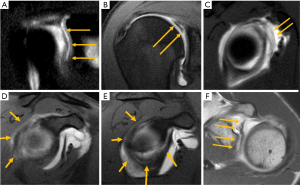
Hill-Sachs lesion occurs simultaneously with glenoid bone lesion in up to 62% of patients with glenohumeral instability (21). These combined injuries have been called bipolar bone lesions (22). Large humeral head Hill-Sachs lesions may cause engagement of the defect with the anterior labrum even after anterior glenoid reconstruction and, therefore, are indication for surgical repair (18). The prevalence of engaging Hill-Sachs lesion is about 7% (22). Typically, an engaging Hill-Sachs has an oblique long axis in neutral shoulder position that become parallel to the anterior edge in ABER position (abduction of 90° and external rotation of more than 30°). When the lesion has a vertical long axis in neutral shoulder position, it runs more diagonally with regard the anterior glenoid in ABER position, and have no tendency to engage (23) (Figure 5). It is also important the theory of glenoid track, defined as the contact area of the posterosuperior humeral head with the glenoid when the arm is raised in ABER position. The width of the glenoid track has been reported to be around 83–85% of the glenoid width (22). If the medial border of a Hill-Sachs lesion is lateral to the glenoid track, there is bone support adjacent to the Hill-Sachs lesion and the lesion is considered “on track” and will not engage; if the medial border of the Hill-Sachs lesion overpasses the glenoid track, there is no humeral bone support enough and the lesion is considered “off track” and will engage (22) (Figure 6).

Several measurements can be used to quantify bone loss in Hill-Sachs lesions. These include humeral residual articular arc and percentage of articular arc loss, with and depth of the lesion on the axial and coronal planes (24) (Figure 6). Of them, the articular arc loss, Hill Sachs lesion width and depth on the axial plane showed greater reliability and are recommended (25). Measurements in the coronal plane showed lower inter-examiner reliability and are less advisable (26). Nevertheless, there is not a universally accepted measurement method to quantify humeral bone loss. Traditionally, lesions involving <20% of the articular surface of the humeral are seldom of clinical significance, whereas lesions >40% tend to be clinically significant and associated to recurrent instability. Others factors should be considered in mid-size lesions comprising 20% to 40% of articular surface in order to choose the appropriate treatment (27).
CT arthrography has also been shown to be accurate in detection of labroligamentous, cartilaginous, and osseous injuries related to anterior shoulder instability, with sensitivities ranging from 82% to 100% and specificities ranging from 96% to 100% (28). Nevertheless, arthro-MRI is mostly used for this purpose.
MRI
MRI is the ultimate tool in assessing shoulder instability. Direct MR arthrography is the standard of care for assessment of shoulder instability in patients younger than 40 years. Shoulder stabilization transfers from the labrum to the rotator cuff with advancing years, limiting the value of arthrography in older patients (29).
In patients younger than 40 years, labral injuries have been described in 39% of patients suffering of shoulder instability and in 19% without instability (28). MR arthrography is the most accurate method for diagnosing the labral tears, reaching a specificity of 93% and sensitivity of 88% based on an arthroscopic reference standard (30). Accurate preoperative classification of the labroligamentous injuries is important, as the type of surgical intervention is dependent on the type of injury.
Glenohumeral instability has been classified into several groups: traumatic (anterior or posterior), atraumatic and minor shoulder instability (31).
Traumatic anterior instability
It is recognized by the acronyms TUBS, for traumatic, unidirectional, Bankart lesion and surgery. It may be anterior or posterior.
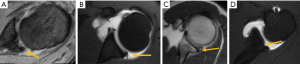
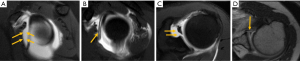
Anterior dislocation is by far more common. 86% of patients with acute anterior instability had been arthroscopically proven to have Bankart lesions (32). It consists of avulsion of the inferior labral complex from the glenoid rim, with complete scapular periosteal disruption. Sometimes is associated with an avulsed fragment of the glenoid rim (osseous Bankart). Accurate measurement of the glenoid bone loss is essential for surgical planning. Small bone gaps can be managed with soft-tissue repair (Bankart procedure). Defects greater than 6 to 8 mm, or superior to 20% to 25%, of the inferior glenoid width usually require bony repair (e.g., Latarjet procedure) (23) (Figure 7).
Several variants of Bankart lesion have been described. In Perthes lesion, avulsion of the anteroinferior labrum is associated with stripped but intact periosteum (33). It is present in 17.9% of patients with acute instability and in 4% of those with chronic instability (32). Perthes lesions are quite often difficult to be detected at both MR imaging and arthroscopically, since the torn labrum may remain in normal or quasi normal position. Imaging in the ABER position puts the anterior band of the inferior glenohumeral ligament (IGHL) and anteroinferior capsule under stress, improving detection rates (34).
ALPSA lesion (anterior labral periosteal sleeve avulsion) is a Bankart variant. It consists of complete disruption of the anteroinferior labrum with medial displacement and inferior rotation of the torn fragment. There is periosteal stripping, but no frank detachment. It is more frequent on chronic and recurrent instabilities of the shoulder, 31%, than in acute anterior instability, 12.5% (32).
GLAD lesions consist of a superficial anterior inferior labral tear with an associated articular cartilage injury. Because the anterior fibers of the IGHL remain attached to glenoid and labrum, it manifests clinically with pain in the anterior aspect of the shoulder, but no signs of anterior instability. In total, 46% of patients with instability and a labral tear had chondral injury, while only 7% of unstable patients without labral tear had a chondral lesion (35).
Up to 9% of patients who underwent surgical intervention for anterior shoulder instability have got an associated humeral avulsion of glenohumeral ligament (HAGL) (36) (Figure 8). Ligament failure occurs at the glenoid labral insertion in 40% of cases, intrasubstance in 35%, and at the humeral insertion in 25% of patients (37). Up to 20% of HAGL lesions demonstrate osseous avulsion from the medial cortical bone of the humeral neck, and when combined with a Bankart lesion are often termed a “floating” IGHL (38). Oblique coronal MR images often show avulsion of the IGHL from the medial humeral attachment, which leads the detached stump of the IGHL band to fall inferiorly, transforming the normal U-shaped appearance of the IGHL into a J shaped structure (39). Further, studies have shown high risk of associated injuries, the most common being the subscapularis tears, which were seen in 68% of patients with HAGL lesions (40,41). HAGL lesions were identified in 21% of arthrographic MR imaging studies at baseline (within 7 days of dislocation), compared with only 7.1% at follow-up (21–54 days) (42).
Traumatic posterior instability
Only 2% of unstable shoulders are attributed to posterior instability, with posterior subluxation being the most common (43), but they are frequently missed. In athletes, sports related posterior “macroinstability” is very rare, although in American football players is almost 15 times more common than in the general population (44). A football lineman might get injured this way, by blocking another player with an extended arm (45). The spectrum of posterior labrum injury includes non-detached tear, crushed or frayed labrum, and detached tear (46).
Reverse Bankart lesions occur when the posterior portion of the glenoid labrum is avulsed during a posterior shoulder dislocation. When this lesion is present, administered contrast can be seen entering into the posterior glenoid fossa, beyond the labrum. Anteriorly, a reversed Hill-Sachs lesion can be found medial to the lesser tuberosity.
When the posterior periosteum is partially avulsed and the labrum medially displaced results in a POLPSA lesion (posterior labro-scapular sleeve avulsion) (47). Kim lesion is an incomplete and concealed superficial tear in the posterior glenoid labrum, usually associated with loss of glenoid labrum’s height and abnormal contour. Failure to identify and treat this lesion leads to permanent posterior instability (48). GARD lesion (the Glenoid Rim Articular Divot lesion) is an impaction injury affecting the posterior glenoid rim, glenoid cavity, or both. Like anterior GLAD injury, it is not associated with instability. Chondral loose bodies may be found (Figure 9).
Similar to HAGL in anterior shoulder dislocation, posterior HAGL (PHAGL) may occur during posterior shoulder dislocation (Figure 8). Chronic traction of the posterior capsule may lead to calcification at the posterior glenoid insertion, known as Bennet disease.
Multidirectional instability (MDI)
It is recognized by the acronyms AMBRII (atraumatic, multidirectional, bilateral, responds to rehabilitation, inferior capsular shift, and interval closure). Most frequent in people less than 35 years old, MDI includes abnormal motion of the shoulder in 2 or 3 planes, usually anterior–inferior and posterior–inferior (49).
The two main anatomic lesions associated with MDI are failure of the rotator cuff interval and laxity of the inferior capsular pouch (Figure 9). The joint capsule at the interval includes the superior glenohumeral ligament and the coracohumeral ligament. With the arm in a neutral position, the coracohumeral and superior glenohumeral ligaments limit inferior translation and external rotation (49). Statistically significant differences in the size and volume of the rotator interval between asymptomatic individuals and those with shoulder instability have been reported (50).
Generally, shoulder instability is inferior with an anterior or posterior component, almost never including all 3 of them. Neer and Foster described three groups of patients based on direction: anteroinferior dislocations and posterior subluxations, posteroinferior dislocations and anterior subluxation and dislocations in all three directions (49). In athletes, there may be associated different types of labral tears and rotator cuff injuries.
Minor shoulder instability
The patients present shoulder pain secondary to shoulder laxity, but TUBS and AMBRII have been excluded. It includes AIOS (acquired instability, overstressed shoulder) and AMSI (atraumatic minor shoulder instability).
Acquired instability secondary to overuse in sport or work activities requires repetitive movements over the shoulder level resulting in injury of capsular structures. It is usually unilateral, in the dominant shoulder, and consists of a microinstability pattern that may led to labral injuries, including superior labral tear from anterior to posterior (SLAP), capsular fibrosis or calcification, and tears of the rotator cuff secondary to internal impingement (51).
An SLAP tear originates at the superior labral site of attachment of the long head of the biceps tendon; however, it can extend to the anterior or posterior portion of the labrum and into adjacent structures (52). Although 4 typed were initially described (Figure 10), nowadays up 10 types are recognized, although most of these represents a combination of type II SLAP with more extensive injuries to the inferior labrum, to the middle or superior glenohumeral ligaments (53) (Figure 11). SLAP lesions were detected in 26% of 544 consecutive shoulder arthroscopies (54).
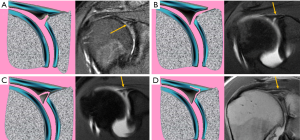
Thickened posterior capsule is commonly seen on imaging of patients with superior labral injuries (55). The GIRD lesion refers to glenoid internal rotation deficit and it is secondary to tightness of the posteroinferior capsule and IGHL as a result of repetitive follow through motions after throwing. MRI may show this thickening of the posterior capsule. When there is a periosteal calcification at the posterior capsular insertion of the posterior inferior glenoid this is called Bennett lesion. It is frequently associated with tears of the posterior labrum, infraspinatus and teres minor tendons (56).
AMSI is a rare condition. Patients refer shoulder pain after a period of inactivity such as pregnancy or immobilization. No generalized joint laxity is present, although microinstability is present because of overload of congenital insufficient static stabilizers associated to muscle atrophy after immobilization. An insufficient, stretched or loose middle glenohumeral ligament (MGHL) may be the only pathology. Anatomic variants of MGHL (absence, hypoplasia, large sublabral foramen or Buford complex) can be present. In Buford complex, anterosuperior labrum is absent in the 1–3 o’clock position and the MGHL is thickened or cord-like, while that in sublabral foramen there is an unattached anterosuperior labrum at the 1–3 o’clock position. Fraying and loosening of these structures may suggest that these anatomic variants are associated to microinstability (Figure 12).
Conclusions
Advances in imaging techniques allow radiologist to achieve a detailed piece of information about anatomic predisposing factors or sequels in shoulder instability. A thorough knowledge of the anatomy of the shoulder, location and types or injures facilitates classification and quantification of these lesions that influence therapeutic selection. In this review, we have seen the main contributions of radiography, CT and MRI in the clinical scenarios of shoulder instability, classified as TUBS (traumatic, unidirectional, Bankart lesion, surgery), AMBRII (atraumatic, multidirectional, bilateral, rehabilitation, inferior capsular shift, interval closure) and “minor shoulder instability”, that includes two entities known as AIOS (acquired instability, overstressed shoulder) and AMSI (atraumatic minor shoulder instability).
Acknowledgements
Thanks to Loreto Vasquez for her kind collaboration reviewing the English grammar of the article.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mazzocca AD, Brown FM Jr, Carreira DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med 2005;33:52-60. [Crossref] [PubMed]
- Matsen FA, Thomas SC, Rockwood CA, Wirth MA. Glenohumeral instability. In: Rockwood CA, Matsen FA. editors. The shoulder. Philadelphia: WB Saunders, 1990:256.
- Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg 2000;9:470-4. [Crossref] [PubMed]
- Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am 1984;66:159-68. [Crossref] [PubMed]
- Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy 2007;23:985-90. [Crossref] [PubMed]
- Lippitt SB, Harryman DT II, Sidles JS, Matsen FA III. Diagnosis and management of AMBRI syndrome techniques. Tech Orthop 1991;6:61-73. [Crossref]
- Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am 1984;66:159-68. [Crossref] [PubMed]
- Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The dead arm revisited. Clin Sports Med 2000;19:125-58. [Crossref] [PubMed]
- Castagna A, Grasso A, Vinanti G. Minor shoulder instability. In: Lajtai G, Snyder SJ, Applegate GR, Aitzmuller G, Gerber C. editors. Shoulder arthroscopy and MRI technique. Berlin: Springer-Verlag, 2003:193-212.
- Pavlov H, Warren RF, Weiss CB Jr, Dines DM. The roentgenographic evaluation of anterior shoulder instability. Clin Orthop Relat Res 1985.153-8. [PubMed]
- Edwards TB, Boulahia A, Walch G. Radiographic Analysis of Bone Defects in Chronic Anterior Shoulder Instability. Arthroscopy 2003;19:732-9. [Crossref] [PubMed]
- VandenBerghe G, Hoenecke HR, Fronek J. Glenohumeral joint instability: the orthopedic approach. Semin Musculoskelet Radiol 2005;9:34-43. [Crossref] [PubMed]
- Mallon WJ, Bassett FH, Goldner RD. Luxatio erecta: the inferior glenohumeral dislocation. J Orthop Trauma 1990;4:19-24. [Crossref] [PubMed]
- van de Bunt F, Pearl ML, Lee EK, Peng L, Didomenico P. Glenoid version by CT scan: an analysis of clinical measurement error and introduction of a protocol to reduce variability. Skeletal Radiol 2015;44:1627-35. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging hill-sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002;18:488-91. [Crossref] [PubMed]
- Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy 2004;20:169-74. [Crossref] [PubMed]
- Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB, LeClere L, Romeo AA. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am 2010;92:133-51. [Crossref] [PubMed]
- Saliken DJ, Bornes TD, Bouliane MJ, Sheps DM, Beaupre LA. Imaging methods for quantifying glenoid and Hill-Sachs bone loss in traumatic instability of the shoulder: a scoping review. BMC Musculoskeletal Disorders 2015;16:164. [Crossref] [PubMed]
- Milano G, Grasso A, Russo A, Magarelli N, Santagada DA, Deriu L, Baudi P, Bonomo L, Fabbriciani C. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med 2011;39:1870-6. [Crossref] [PubMed]
- Widjaja AB, Tran A, Bailey M, Proper S. Correlation between bankart and hill-sachs lesions in anterior shoulder dislocation. ANZ J Surg 2006;76:436-8. [Crossref] [PubMed]
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy 2014;30:90-8. [Crossref] [PubMed]
- Pouliart N, Doering S, Shahabpour M.. What can the Radiologist do to help the Surgeon Manage Shoulder Instability? J Belg Radiol 2016;100:1-13.
- Cho SH, Cho NS, Rhee YG. Preoperative analysis of the Hill-Sachs lesion in anterior shoulder instability: how to predict engagement of the lesion. Am J Sports Med 2011;39:2389-95. [Crossref] [PubMed]
- Assunção JH, Conforto Gracitelli ME, Dias Borgo G, Malavolta EA, Bordalo-Rodrigues M, Ferreira Neto AA. Tomographic evaluation of Hill-Sachs lesions: is there a correlation between different methods of measurement? Acta Radiologica 2017;58:77-83. [Crossref] [PubMed]
- Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. J Shoulder Elbow Surg 2011;20:1328-34. [Crossref] [PubMed]
- Provencher MT, Frank RM, LeClere LE, Metzger PD, Ryu JJ, Bernhardson LT, Romeo AA. The Hill-Sachs Lesion: Diagnosis, Classification, and Management. J Am Acad Orthop Surg 2012;20:242-52. [Crossref] [PubMed]
- Acid S, Le Corroller T, Aswad R, Pauly V, Champsaur P. Preoperative imaging of anterior shoulder instability: diagnostic effectiveness of MDCT arthrography and comparison with MR arthrography and arthroscopy. AJR Am J Roentgenol 2012;198:661-7. [Crossref] [PubMed]
- Rowan KR, Keogh C, Andrews G, Cheong Y, Forster BB. Essentials of shoulder MR arthrography: a practical guide for the general radiologist. Clin Radiol 2004;59:327-34. [Crossref] [PubMed]
- Smith TO, Drew BT, Toms AP. A metaanalysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg 2012;132:905-19. [Crossref] [PubMed]
- Castagna A, Nordenson U, Garofalo R, Karlsson J.. Minor shoulder instability. Arthroscopy 2007;23:211-5. [Crossref] [PubMed]
- Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 2005;237:578-83. [Crossref] [PubMed]
- Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR Am J Roentgenol 2002;178:233-7. [Crossref] [PubMed]
- Tian CY, Cui GQ, Zheng ZZ, Ren AH. The added value of ABER position for the detection and classification of anteroinferior labroligamentous lesions in MR arthrography of the shoulder. Eur J Radiol 2013;82:651-7. [Crossref] [PubMed]
- O’Brien J, Grebenyuk J, Leith J, Forster BB. Frequency of glenoid chondral lesions on MR arthrography in patients with anterior shoulder instability. Eur J Radiol 2012;81:3461-5. [Crossref] [PubMed]
- Magee T.. Prevalence of HAGL lesions and associated abnormalities on shoulder MR examination. Skeletal Radiol 2014;43:307-13. [Crossref] [PubMed]
- Bigliani LU, Pollock RG, Soslowsky LJ, Flatow EL, Pawluk RJ, Mow VC. Tensile properties of the inferior glenohumeral ligament. J Orthop Res 1992;10:187-97. [Crossref] [PubMed]
- Oberlander MA, Morgan BE, Visotsky JL. The BHAGL lesion: a new variant of anterior shoulder instability. Arthroscopy 1996;12:627-33. [Crossref] [PubMed]
- Carlson CL. The “J” sign. Radiology 2004;232:725-6. [Crossref] [PubMed]
- Bui-Mansfield LT, Taylor DC, Uhorchak JM, Tenuta JJ. Humeral avulsions of the glenohumeral ligament: imaging features and a review of the literature. AJR Am J Roentgenol 2002;179:649-55. [Crossref] [PubMed]
- Tirman PFJ, Steinbach LS, Feller JF, Stauffer AE. Humeral avulsion of the anterior shoulder stabilizing structures after anterior shoulder dislocation: demonstration by MRI and MR arthrography. Skeletal Radiol 1996;25:743-48. [Crossref] [PubMed]
- Liavaag S, Stiris MG, Svenningsen S, Enger M, Pripp AH, Brox JI. Capsular lesions with glenohumeral ligament injuries in patients with primary shoulder dislocation: magnetic resonance imaging and magnetic resonance arthrography evaluation. Scand J Med Sci Sports 2011;21:e291-7. [Crossref] [PubMed]
- Millett PJ, Clavert P, Hatch GF 3rd, Warner JJ. Recurrent posterior shoulder instability. J Am Acad Orthop Surg 2006;14:464-76. [Crossref] [PubMed]
- Escobedo EM, Richardson ML, Schulz YB, Hunter JC, Green JR 3rd, Messick KJ. Increased risk of posterior glenoid labrum tears in football players. AJR Am J Roentgenol 2007;188:193-7. [Crossref] [PubMed]
- VandenBerghe G, Hoenecke HR, Fronek J. Glenohumeral Joint Instability: The Orthopedic Approach. Semin Musculoskelet Radiol 2005;9:34-43. [Crossref] [PubMed]
- Shah N, Tung GA. Imaging signs of posterior glenohumeral instability. AJR Am J Roentgenol 2009;192:730-5. [Crossref] [PubMed]
- Yu JS, Ashman CJ, Jones G. The POLPSA lesion: MR imaging findings with arthroscopic correlation in patients with posterior instability. Skeletal Radiol 2002;31:396-9. [Crossref] [PubMed]
- Kim SH, Ha KI, Yoo JC, Noh KC. Kim's lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy 2004;20:712-20. [Crossref] [PubMed]
- Neer CS 2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am 1980;62:897-908. [Crossref] [PubMed]
- Kim KC, Rhee KJ, Shin HD, Kim YM. Estimating the dimensions of the rotator interval with use of magnetic resonance arthrography. J Bone Joint Surg Am 2007;89:2450-5. [PubMed]
- Woertler K, Waldt S.. MR imaging in sports-related glenohumeral instability. Eur Radiol 2006;16:2622-36. [Crossref] [PubMed]
- Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy 1990;6:274-9. [Crossref] [PubMed]
- Chang D, Mohana-Borges A, Borso M, Chung CB. SLAP lesions: Anatomy, clinical presentation, MR imaging diagnosis and characterization. Eur J Radiol 2008;68:72-87. [Crossref] [PubMed]
- Kim TK, Queale WS, Cosgarea AJ, McFarland EG. Clinical features of the different types of SLAP lesions: an analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am 2003;85-A:66-71. [Crossref] [PubMed]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy 2003;19:531-9. [Crossref] [PubMed]
- Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: the Bennett lesion. Etiology, diagnosis, and treatment. Am J Sports Med 1994;22:171-5. [Crossref] [PubMed]


