Mucoepidermoid carcinoma of the trachea
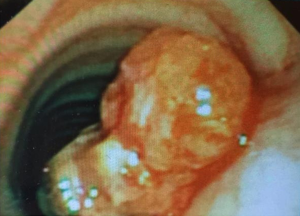
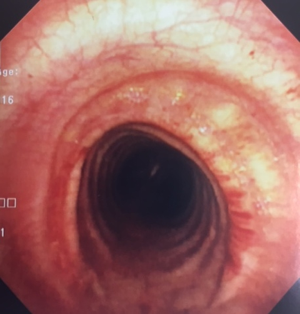
A 24-year-old gentleman, previously medically free, presented with symptoms of cough and intermittent hemoptysis for several weeks. Laboratory work up was within normal limits. CT-scan of the neck and chest was done and revealed a 1.5×1.5×0.9 cm lobulated intraluminal tracheal mass arising from the posterior tracheal wall at the level of upper manubrium, with possible invasion of mediastinal fat posterior to the tracheal wall. There was no evidence of lymphadenopathy. Flexible bronchoscopy showed a large tracheal tumor (Figure 1) obstructing 60–70% of the trachea. Needle biopsy revealed low-grade mucoepidermoid carcinoma (Figure 2).
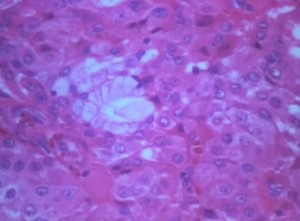
The patient underwent open partial tracheal resection and reconstruction under rigid bronchoscopy guidance. No further therapy was provided, and he remained asymptomatic on subsequent follow up. A 2-year post resection surveillance bronchoscopy of the surgical site is shown (Figure 3).
Primary salivary-gland tumors of the lung are extremely rare, comprising only 0.1–0.2% of primary lung cancers and less than 1% of primary malignant bronchial tumors. Mucoepidermoid carcinoma (MEC) is a salivary-gland type of lung cancer that originates from the submucosal glands of the tracheobronchial tree. It affects patients of age 30 years and older (1,2).
Patients may present with symptoms of bronchial irritation including cough, hemoptysis, wheezing and post-obstructive pneumonia, but may also be asymptomatic (1,2).
MEC is classified as low-grade or high-grade based on histologic appearance.
Surgical resection is the mainstay of treatment, and usually carries good prognosis. Low-grade malignant tumors of the bronchial airway are often managed with open resection. High-grade MEC carries a higher risk of distant metastasis and worse prognosis even with surgery (2,3).
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abu Saleh WK, Aljabbari O, Ramchandani M. Mucoepidermoid Carcinoma of the Tracheobronchial Tree. Methodist Debakey Cardiovasc J 2015;11:192-4. [Crossref] [PubMed]
- Shen C, Che G. Clinicopathological analysis of pulmonary mucoepidermoid carcinoma. World J Surg Oncol 2014;12:33. [Crossref] [PubMed]
- Kawano O, Yuki D, Fukai I, et al. Successful treatment of mucoepidermoid carcinoma in the left main bronchus. Surg Case Rep 2015;1:85. [Crossref] [PubMed]