Main pulmonary artery trifurcation in association with persistent right common pulmonary vein: a piece of embryological puzzle
Introduction
Wide variety of congenital anomalies of pulmonary arteries like pulmonary stenosis, pulmonary atresia, proximal interruption, anomalous origin of left pulmonary artery (LPA) and idiopathic dilatation of pulmonary trunk are described in the literature (1,2). Few studies have also described the variations in pulmonary artery branching pattern, mainly describing anomalies of lobar and segmental branching pattern (3,4). Combination of ipsilateral arterial and venous anomaly is relatively uncommon. We present a unique case of main pulmonary artery (MPA) trifurcation into LPA, right upper and lower lobar pulmonary arteries with associated persistent right common pulmonary vein (rCPV). We review the embryology and propose an embryological explanation to this rare anatomical variation.
Case presentation
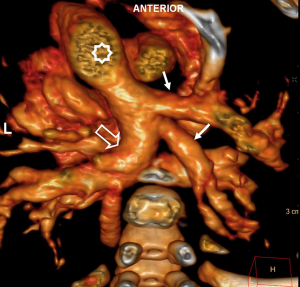
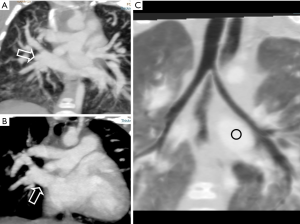
A 5-month-old female child was brought to the hospital with features of anorectal malformation. On presurgical screening evaluation and echocardiography, ventricular and atrial septal defects (ASD and VSD) were noted with suspicion of partial resorption of pulmonary veins. Multidetector computed tomography (MDCT) was performed with Philips Ingenuity 128 slice scanner (Koninklijke Philips N.V.) for further anatomical assessment confirmed the ASD and subaortic VSD. It also showed MPA trifurcating into LPA, right upper and right lower lobar pulmonary arteries. Segment of right main pulmonary artery (RPA) was absent with direct origin of lobar branches from MPA (Figures 1,2). There was no evidence of main or branch pulmonary artery stenosis. Examination additionally revealed persistent rCPV formed by the union of right superior and right inferior pulmonary veins (Figure 3A,B) draining to the left atrium (LA). There was indirect evidence of pulmonary arterial hypertension (PAH) in the form of dilated MPA and right heart chambers. Bronchial morphology was left sided with hyparterial bronchus on both sides (Figure 3C).

Discussion
The main pulmonary trunk develops from truncus arteriosus. RPA and LPA are derived from right and left sixth aortic arches. RPA and LPA further communicate with lobar, segmental and sub-segmental branches derived from developing lung buds. Variety of congenital anomalies of pulmonary arteries are described in literature like pulmonary stenosis, pulmonary atresia, proximal interruption of pulmonary artery, anomalous origin of LPA and idiopathic dilatation of pulmonary trunk etc. (1,2). In our case there is trifurcation of MPA wherein there is direct origin of right lobar arteries along with the LPA. This anomaly appears to be due to unusual resorption of segment of RPA resulting in direct communication of MPA to the derivatives of lung buds.
During early development of lung buds, precursors of pulmonary vascular system (arterial and venous) develop along the airways. While arterial components closely approximated with the airways, venous structures are located at a distance. Arterial and venous components develop simultaneously, and arteries are differentiated by the addition of muscular components in the vessel wall from bronchial smooth muscles. Beyond 28 days and subsequently, in the phase of vasculogenesis, differentiated arterial and venous structures establish communication with the elements of 6th bronchial arch, which in turn are connected to pulmonary arteries derived from the division of truncus arteriosus. Observations in our patient suggest that there is predominant contribution of vascular components from the right lung bud in the development of right pulmonary artery and vein, thus explaining absent proximal pulmonary component from 6th arch and early division of RPA (5). Generally development of pulmonary veins starts around 27–29 days of gestational age when a small endothelial outgrowth occurs from posterior LA wall, known as common pulmonary vein (CPV). CPV further divides into right and left branches. As the LA starts growing, the CPVs on either side gradually get absorbed into the LA, resulting in four separate veins opening into LA (6,7). In our case there appears to be incomplete absorption of CPV into LA leading to persistent rCPV. This observation fits into tubular form of cor triatriatum as described in earlier studies (8). Variation in the development of venous component from lung bud may also have some contribution to the persistence of ipsilateral CPV. Incidentally it may be noted that persistent CPV is more common on the left side rather than right, whereas multiple pulmonary veins of more frequent on the right side (5).
Anomaly noted in our patient becomes significant when it occurs in congenital heart disease wherein surgical systemic-pulmonary shunt is envisaged. It is an observation of significance when planning pneumonectomy and endarterectomy of pulmonary arteries.
To the best of our knowledge this is the first case description of MPA trifurcation in association with persistent rCPV. We propose that likely embryological basis of this anomaly is primarily related to simultaneously occurring variations in the extent of vasculogenesis of lung bud, development of RPA from 6th aortic arch and their integration. The same mechanism may be playing a role in related ipsilateral pulmonary venous anomaly.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Castañer E, Gallardo X, Rimola J, Pallardó Y, Mata JM, Perendreu J, Martin C, Gil D. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. Radiographics 2006;26:349-71. [Crossref] [PubMed]
- Carter BW, Lichtenberger JP 3rd, Wu CC. Congenital abnormalities of the pulmonary arteries in adults. AJR Am J Roentgenol 2014;202:W308-13. [PubMed]
- Wells TR, Takahashi M, Landing BH, Ritchie GW, Ang SM, Diaz JF, Mahnovski V. Branching patterns of right pulmonary artery in cardiovascular anomalies. Pediatr Pathol 1993;13:213-23. [Crossref] [PubMed]
- Murota M, Satoh K, Yamamoto Y, Kobayashi T, Nishiyama Y. Evaluation of subsubsegmental pulmonary arteries of the posterior and anterior segments of the right upper lobe using multidetector row computed tomography with multiplanar reconstruction images. Jpn J Radiol 2009;27:86-90. [Crossref] [PubMed]
- Hislop AA. Airway and blood vessel interaction during lung development. J Anat 2002;201:325-34. [Crossref] [PubMed]
- Vyas HV, Greenberg SB, Krishnamurthy R. MR imaging and CT evaluation of congenital pulmonary vein abnormalities in neonates and infants. Radiographics 2012;32:87-98. [Crossref] [PubMed]
- NEILL CA. Development of the pulmonary veins; with reference to the embryology of anomalies of pulmonary venous return. Pediatrics 1956;18:880-7. [PubMed]
- Hoeffel JC, Pernot C, Worms AM, Luceri R. Persistence of the common pulmonary vein in a child. AJR Am J Roentgenol 1979;133:121-2. [Crossref] [PubMed]


