Imaging evaluation of catheter integrity prevent potentially fatal complication of pinch-off syndrome: illustration of two cases
Introduction
Peripherally inserted central catheters (PICC) and implantable venous access devices with an attached catheter such as a Port-A-Cath are common types of central venous catheters (CVC) that are used to deliver chemotherapy and other medications. Subclavian vein (SVC) access for CVC, although widely practiced, presents risks for catheter complications such as the compression of the catheter in the space anterior to the first rib and posterior to the clavicle (1). This compression is rated on a scale of grades 0 to 3 pinch-off syndrome (POS). Grade 0 exhibits a regular catheter course without luminal narrowing; grade 1 exhibits an altered catheter course without luminal narrowing; grade 2 exhibits luminal narrowing; and grade 3 exhibits catheter fracture (2). POS may present with pain or swelling of the shoulder region but patients may also be asymptomatic (3). Additionally, POS can be an incidental finding seen on a chest X-ray (4). Regardless, clinicians should suspect a possible POS if there is patient-reported pain or an abnormal catheter pathway seen on a chest X-ray. Further investigation via radiographic or fluoroscopic evaluation is warranted. Early detection of POS requires only catheter replacement but failure to intervene may result in life-threatening complications caused by catheter fragmentation. In such cases, pieces of the catheter may break off to cause ventricular tachycardia, vessel embolization, and cardiac perforation (5-7). In this report, we discuss two cases of grade 3 POS that were detected based on clinical and radiographic signs.
Case presentation
Case 1
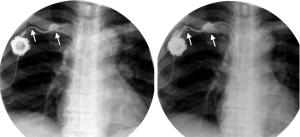
A 63-year-old female with pancreatic carcinoma metastatic to her liver underwent placement of a Port-A-Cath (Vortex VX Port with an 8 French CVC) via the right SCV (Figure 1). She experienced swelling and pain in the soft tissues surrounding the port reservoir and along the catheter’s course at her last chemotherapy infusion. Aspiration of the port was noted to be difficult. Upon fluoroscopic examination, contrast injection demonstrated two breaks: one 2 cm from the connection to the port reservoir and a larger break near the subclavian access site between the first rib and the clavicle (Figure 2). Based on the fluoroscopic evidence of breaks in the catheter, grade 3 POS was confirmed. The Port-A-Cath was replaced with a new 8 French catheter and port. Aspiration of the new port proved patency, and the patient was discharged.
Case 2
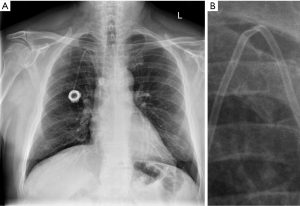
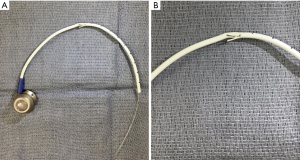
A 66-year-old male with diffuse large B-cell lymphoma underwent a pre-allogenic stem cell transplant work-up. He had an 8 French Port-A-Cath through his right SCV for chemotherapy infusion. Chest X-ray demonstrated an abnormal kink at the apex of the catheter route from the SCV to the azygos vein (Figure 3A,B). Based on the catheter kink shown on the chest X-ray, grade 2 or 3 POS was suspected. Difficulty with aspiration of the port combined with pain in the shoulder area caused the interventional radiologist to immediately retrieve the catheter. The extracted catheter exhibited significant damage to the wall that exposed the catheter lumen (Figure 4A,B). These findings confirmed a grade 3 POS. A new PICC was placed through the right SCV and tested for patency. After the successful replacement of the Port-A-Cath, the patient was discharged.
Discussion
CVC associated POS is a serious complication. Due to POS, a compromised catheter can leak, and pieces of a broken-off catheter can travel through the vascular network. These catheter fragments can cause life-threatening complications such as ventricular tachycardia, vessel embolization, and cardiac perforation (5-7). In Fisher et al.’s review regarding fractured catheters, 71% of these cases resulted in serious complications or death (8).
POS manifests with physical signs and notable features on radiographic and fluoroscopic imaging which allow for early detection before serious complications arise. Because CVCs are regularly used to deliver chemotherapeutics, POS can present with pain, swelling, and tissue necrosis from inappropriate leakage of the infusions into surrounding tissue. In addition, POS can cause difficulty in aspirating or flushing the CVC prior to an infusion session. Relieving these signs of obstruction by raising the arm on the side of the CVC or by rolling the corresponding shoulder is a hallmark of POS. It is important to note that symptoms of POS appear earlier in high-volume or continuous infusion catheters versus low-volume or intermittent catheters (1).
Suspected POS catheters are often evaluated with a chest X-ray or fluoroscopic imaging. On a chest X-ray, a catheter affected by POS may display a kink as seen in our second case, an abnormally sharp turn, or in severed pieces (3,4,7). The findings can often be incidental as some patients with POS may be asymptomatic (4). Fluoroscopic evaluation of a suspected catheter usually involves the injection of intravenous contrast to identify any areas of leakage as was seen in our first case. Any contrast leakage would suggest a grade 3 POS.
The management of POS requires the immediate removal of the compromised catheter if grade 2 or 3 POS is suspected (2). This entails a simple retrieval of the catheter from the insertion site. For fragmented catheters, percutaneous transcatheter retrieval of the fragments with a loop snare can be done under fluoroscopic guidance and mild anesthesia (5,7,8). A repeat X-ray should be taken after the retrieval to confirm there are no catheter fragments remaining. Grade 0 or 1 POS is of little clinical significance but should be monitored routinely for any changes (2).
For optimal SCV placement that avoids POS, the catheter insertion site should be as lateral as possible. Ultrasound guidance has been shown to help clinicians place SCV catheters more laterally, thus preventing POS (9). Additionally, compared to the SCV, studies have shown that the internal jugular vein (IJV) insertion site for implantable venous devices has lower rates of venous thrombosis, catheter malfunction, and catheter malposition (10). Although many surgeons, interventional radiologists, and other clinicians historically prefer the SVC as insertion sites for CVCs, the use of the right IJV access site can aid in reducing the occurrence of POS and its associated serious complications.
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Andris DA, Krzywda EA, Schulte W, Ausman R, Quebbeman EJ. Pinch-off syndrome: a rare etiology for central venous catheter occlusion. JPEN J Parenter Enteral Nutr 1994;18:531-3. [Crossref] [PubMed]
- Hinke DH, Zandt-Stastny DA, Goodman LR, Quebbeman EJ, Krzywda EA, Andris DA. Pinch-off syndrome: a complication of implantable subclavian venous access devices. Radiology 1990;177:353-6. [Crossref] [PubMed]
- Cho JB, Park IY, Sung KY, Baek JM, Lee JH, Lee DS. Pinch-off syndrome. J Korean Surg Soc 2013;85:139-44. [Crossref] [PubMed]
- Mery M, Palengat S, Loffroy R, Vernet M, Matet P, Cherblanc V. Fracture and atypical migration of an implantable central venous access device. Quant Imaging Med Surg 2016;6:312-4. [Crossref] [PubMed]
- Biswas S, McNerney P. Ventricular Tachycardia from a Central Line Fracture Fragment Embolus: A Rare Complication of a Commonly Used Procedure-A Case Report and Review of the Relevant Literature. Case Rep Crit Care 2015;2015:265326. [Crossref] [PubMed]
- Monsuez JJ, Douard MC, Martin-Bouyer Y. Catheter fragments embolization. Angiology 1997;48:117-20. [Crossref] [PubMed]
- Ghaderian M, Sabri MR, Ahmadi AR. Percutaneous retrieval of an intracardiac central venous port fragment using snare with triple loops. J Res Med Sci 2015;20:97-9. [PubMed]
- Fisher RG, Ferreyro R. Evaluation of current techniques for nonsurgical removal of intravascular iatrogenic foreign bodies. AJR Am J Roentgenol 1978;130:541-8. [Crossref] [PubMed]
- Tamura A, Sone M, Ehara S, Kato K, Tanaka R, Nakasato T, Itabashi T. Is ultrasound-guided central venous port placement effective to avoid pinch-off syndrome? J Vasc Access 2014;15:311-6.
- Araújo C, Silva JP, Antunes P, Fernandes JM, Dias C, Pereira H, Dias T, Fougo JL. A comparative study between two central veins for the introduction of totally implantable venous access devices in 1201 cancer patients. Eur J Surg Oncol 2008;34:222-6. [Crossref] [PubMed]



