Two cases of tuberculous spondylodiscitis: a rare manifestation of extrapulmonary tuberculosis
Introduction
Osteoarticular manifestations of tuberculosis are the third manner of presentation of extrapulmonary tuberculosis with a frequency less than 5%, being the main site affected the axial skeleton. This is known as tuberculous spondylodiscitis or Pott’s disease, preferably appearing in the dorsal region (1,2). Pott’s disease was first described in 1799 by Percivall Pott as “That kind of palsy of lower limbs witch is frequently found to accompany a curvature of the spine”; but it is known to be one of the oldest diseases to mankind dating back to Egyptian mummies in 3400 BC. It is the most common granulomatous disease of the spine, which is characterized by being chronic and slowly progressive, to its confirmation Mycobacterium tuberculosis isolation or identification of granulomas in a sample obtained from the injured vertebrae is needed (2,3). Imaging studies are important for diseases detection, mainly the computed axial tomography (CT) and magnetic resonance imaging (MRI) which since 1987 have made it possible to detect the disease at a predestructive phase and at rare sites of presentation (1,2). Treatment involves the use of antituberculosis drugs for at least 6 months, and surgery was reserved for cases with progressive deformity or neurological deficit in which medical treatment is not effective, which represents one-third of patients (1,3,4). In the search made in PubMed database there were scarce cases with the same characteristics (5,6). In this report we represent two cases of tuberculous spondylodiscitis.
Case presentation
Case 1
One male patient of 22 years old with a history of exposure to fuel particulate matter air pollution of 264 hours/year, with positive exposure to tuberculosis as his father has this disease. He started symptoms 2 months before the admission at the clinics with pleuritic pain in the posterior thorax, which was intensified with deep breathing, partially (decreasing) with the administration of NSAIDs (acetaminifen and diclofenac), adding paresthesia and dysesthesia in the left lower limb. Subsequently he presented morning fever quantified up to 38.8 °C, sweats and chills with 1 week of evolution, which did not diminished to antipyretics (acetaminophen and metamizol) finally showed paraparesis and decreased sensation in the pelvic limbs, so he went to hospitalization. In the physical examination, decreased muscle strength and tendon reflexes of lower limbs, and sensory level in T6 dermatome were found.
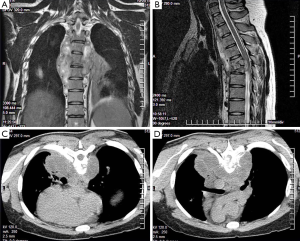
Paraclinical on admission: Hb: 12.3 g/dL, hematocrit: 38%, neutrophils: 3.4×103, lymphocytes: 1.5×103 and serum electrolytes within normal parameters. Chest X-ray result within normal parameters. CT of chest was performed, in which an image hypodense paravertebral between T2–T5 was observed, as well as a destruction of the vertebral bodies of T5 and T6 (Figure 1). Was requested thoracic spine MRI, finding mediastinal tumor involving vertebral bodies T4–T5, with spinal cord compression, in T2 an isointense, paravertebral and bilateral image was observed at T2–T5 level, suggestive of abscess, as well as fracture and collapse of the vertebral body of T5 (Figure 1). Biopsy was performed reporting chronic granulomatous inflammatory lesions with multinucleated giant cells with caseous necrosis without cellular atypia. Ziehl-Neelsen stain was made finding scarce acid-fast bacilli compatible with Mycobacterium tuberculosis. Enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV) was performed with negative results. It was valued by the spinal surgery department that suggested conservative management with permanent Jewett corset till control infection. Management with Dotbal (rifampin, isoniazid, pyrazinamide, ethambutol), two tablets every 12 hours began, completing intensive and supportive phase. The treatment was successful, currently he presents results of the polymerase chain reaction (PCR) for Mycobacterium tuberculosis negative and sensory and motor recovery of the limbs, normal tendon reflexes, he performs physical effort without complications, without the presence of chest pain and also he has remained afebrile.
Case 2
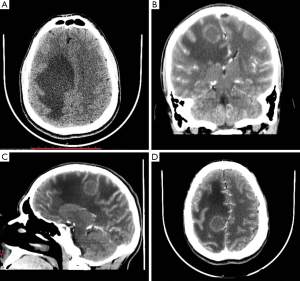
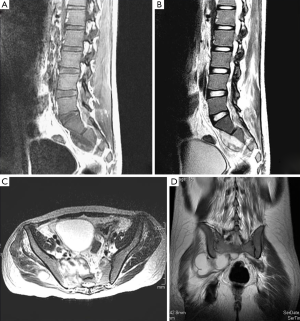
One male patient of 21 years old with a history of alcohol since 15 years old to the present, once a week. He began his current condition 3 months before admission with right hip pain of moderate intensity, with limitation of external rotation, which decreased the administration of analgesics. Showed loss of 15 kg of weight in 6 weeks, then subsequently holocraneal headache not pulsatile, intermittent, which partially decreased due the use of NSAIDs (diclofenac), added to the condition, tonic-clonic movements in the left side of the body, due this he was taken to hospitalization. At admission, the patient was conscious, oriented, referring the presence of holocraneal headache, no data targeting. Paraclinical: Hb: 14.2 g/dL, hematocrit: 41%, neutrophils: 7.2×103, lymphocytes: 2.1×103 cells, glucose 97 mg/dL and serum electrolytes within normal parameters. TAC skull was done, reporting right parasagittal lesion with significant perilesional edema and reinforcement ring, subfalcial hernia and displacement of the midline (Figure 2). He began antibiotic treatment and due not present clinical improvement was evaluated by neurosurgery, who decided abscess drainage. Studies of the sample were conducted, reported negative cultures, Gram stain negative, negative ink, Ziehl-Neelsen stain was made finding scarce acid-fast bacilli compatible with Mycobacterium tuberculosis. ELISA for HIV was performed with negative results. During his recovery he presented again right hip pain with intensity visual analog scale 8/10, with limitation of external rotation, which did not yield to analgesic management, due this MRI was performed, finding pelvic abscess collection compatible with intra-spinal block extension and peripheral soft tissue (Figure 3). Chest radiography was performed, with results within normal parameters. Abscess drainage was performed with Ziehl-Neelsen stain, where acid-fast bacilli were compatibles with Mycobacterium tuberculosis were observed, confirming the diagnosis with culture. Ziehl-Neelsen stain was requested in urine, resulting positive. Management with Dotbal was initiated (rifampin, isoniazid, pyrazinamide, ethambutol) for 12 months due extrapulmonary affectation, which ended without sequelae or complications involvement. Based control PCR for Mycobacterium tuberculosis, gave a negative result. After the successful treatment, the patient has no hip pain or mobility limitation, no headache or hypertensive data skull.
Discussion
We report the cases of two young patients with negative serology for HIV, which were diagnosed with Pott’s disease. Since the advent of HIV, have emerged opportunistic diseases, including tuberculosis, nevertheless extrapulmonary manifestations, such as tuberculous spondylodiscitis, have increased their frequency (7-9). In a study by García-Lechuz et al. (2) in 1,407 patients with the diagnosis of tuberculosis, only 0.9% had Pott’s disease, being 58 years the average age, affecting mainly dorsal level and more frequently in the male gender. With regard to our case studies, age was much lower than that reported by García-Lechuz et al., and one of our patients had lumbosacral injury. Jodra et al. (10) reported a case of Pott’s disease in a young patient, like ours, with involvement at the dorsal level and performing diagnostics with staining Zielhl-Neelsen collection, as in our patients, responding appropriately to management antifimic. Clinical manifestations of tuberculous spondylodiscitis are characterized by nonspecific symptoms, which results in delayed diagnosis; however the symptom that is present in almost all patients (80–100%) is pain at the site level location injury (11). The clinical presentation is associated with systemic disease, as with local injury. Neurological symptoms are second in frequency, as a weakness, paresthesias and paraplegia. Patients often have a chronic course with weight loss in half the cases, the presence of fever, malaise, and night sweats is also common in a third of patients (1,2,11). It is common the presence of comorbidities in these patients, especially those who have a decreased immune response cell type. Increased risk has been observed in patients with diabetes mellitus, HIV infection, kidney or liver failure, obstructive pulmonary disease, chronic corticosteroid use, alcohol consumption and use of immunosuppressive transplanted (2,11). In the case of our two patients, one of them had a history of chronic alcoholism. Similarly, they may have tuberculosis infection in other locations, mainly in the lungs, followed by nodal level, but may also have renal and hepatic affectation (2,11,12). Our patients had no pulmonary tuberculosis, however one of them presented brain abscess secondary to Mycobacterium tuberculosis, which is rare and this combination has not been reported in the literature. Locally they can present paraspinal abscess, epidural or paraspinal psoas (2,11). The diagnosis is usually delayed from 2 months to 2 years, this due to the insidiousness of symptoms as the difficulty of recognizing the spinal injury. Imaging studies are of great importance for the diagnosis, such as plain radiographs in which can be observe the processes of the vertebrae and the loss of its anatomy, the first radiographic sign is osteoporosis of the body affected, followed by osteolysis which can progress to spondylodiscitis (11,13); the axial CT scan allows us to observe the exact extent of bone lesion, lesions within the vertebral body and the presence of invasion of the spinal canal, can be used for diagnosis and monitoring of disease (11-13). In the MRI can be observed osteolytic lesions, disc space narrowing, loss of vertebral body height, erosions in the endplates, the presence of intra and extravertebral abscesses and compression of the dural sac, preferably being the imaging study in this pathology (11,13). It is essential to confirm the presence of the agent, for this can be used intradermal reaction Mantoux (PPD), Ziehl-Neelsen stain, PCR genome of the mycobacterium and quantification of interferon gamma released (11,14). Treatment involves the administration of antifimic drugs for a period of 12 months, being necessary only surgical treatment in a third of patients (1,3,4). Two cases of Pott’s disease were presented, it is well known that the typical presentation is a level dorsal and upper lumbar, sacrum and cervical involvement is uncommon, even so, one of our patients had injury to sacral level. Two cases of Pott’s disease were presented, it is well known that the typical presentation is a level dorsal and upper lumbar, sacrum and cervical involvement is uncommon, even so, one of our patients had injury to sacral level. The classic findings are infection of the intervertebral disc, destruction of two or more continuous vertebras (5), in our first patient, destruction of the fifth and sixth thoracic vertebral body was found, another classic finding is the presence of a paraspinal mass or collection (5) as shown in Figure 1. It is known that atypical presentations are characterized by the absence of lesions to the intervertebral disc (5), so we could say that our cases are atypical presentation. This could be because the disc is avascular, so that infection is observed belatedly. The MRI is the study of choice for the accurate diagnosis of lesions caused by Mycobacterium tuberculosis at the spine level, as was reported in the others similar articles (5,6), likewise can be used in monitoring. It has high sensitivity in detecting changes at the level of the spinal cord and the initial inflammatory changes in the vertebral bodies. Because of this, our patients underwent this study to determine the lesions in the spine level, finding characteristic features as the paravertebral collection, the destruction of the vertebral bodies, however not intervertebral disc injury was found. The importance of our cases lies in the low frequency of presentation in patients without the presence of HIV, as well as presentations at sacral level, has not been found in the literature coexistence between Pott’s disease and the presence of brain abscess caused by Mycobacterium tuberculosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- López-Sánchez MC, Calvo Arrojo G, Vázquez-Rodríguez TR. Tuberculous spondylodiskitis with lumbar tumor. Reumatol Clin 2012;8:292-3. [Crossref] [PubMed]
- García-Lechuz JM, Julve R, Alcalá L, Ruiz-Serrano MJ, Muñoz P. Tuberculous spondylodiskitis (Pott's disease): Experience in a general hospital. Enferm Infecc Microbiol Clin 2002;20:5-9. [Crossref] [PubMed]
- Varatharajah S, Charles YP, Buy X, Walter A, Steib JP. Update on the surgical management of Pott's disease. Orthop Traumatol Surg Res 2014;100:229-35. [Crossref] [PubMed]
- Kandwal P. G V, Jayaswal A. Management of Tuberculous Infection of the Spine. Asian Spine J 2016;10:792-800. [Crossref] [PubMed]
- De Backer AI, Mortelé KJ, Vanschoubroeck IJ, Deeren D, Vanhoenacker FM, De Keulenaer BL, Bomans P, Kockx MM. Tuberculosis of the spine: CT and MR imaging features. JBR-BTR 2005;88:92-7. [PubMed]
- Shen Y, Zhong W, Peng D, Lu C, Xiong G, Li D, Deng Y, Tan L. Atypical, multilevel and noncontiguous tuberculous spondylitis that affected the vertebrae of thoracic, lumbar and sacrum: a case report. Int J Clin Exp Med 2015;8:3006-9. [PubMed]
- Jaeger S, Karargyris A, Candemir S, Siegelman J, Folio L, Antani S, Thoma G. Automatic screening for tuberculosis in chest radiographs: a survey. Quant Imaging Med Surg 2013;3:89-99. [PubMed]
- Wang Y, He G, Zhan W, Jiang H, Wu D, Wang D, Tang A. CT findings in splenic tuberculosis. J Belge Radiol 1998;81:90-1. [PubMed]
- Wang YX, Chen CR, He GX, Tang AR. CT findings of adrenal glands in patients with tuberculous Addison's disease. J Belge Radiol 1998;81:226-8. [PubMed]
- Jodra S, Alvarez C. Images in clinical medicine. Pott's disease of the thoracic spine. N Engl J Med 2013;368:756. [Crossref] [PubMed]
- Trecarichi EM, Di Meco E, Mazzotta V, Fantoni M. Tuberculous spondylodiscitis: epidemiology, clinical features, treatment, and outcome. Eur Rev Med Pharmacol Sci 2012;16 Suppl 2:58-72. [PubMed]
- Graña D, Ponce de León C, Danza Á, Gutiérrez I, Dufrechou C. Espondilodiscitis tuberculosa: uso de los exámenes complementarios con una nueva perspectiva. A propósito de dos casos clínicos y revisión de la literatura. Archivos de Medicina Interna 2015;37:18-22.
- Vergara AC, Barrios PJ, González F. Diagnosis by images of vertebral tuberculosis. A case report. Medisur 2015;13:303-8.
- Delogu G, Zumbo A, Fadda G. Microbiological and immunological diagnosis of tuberculous spondylodiscitis. Eur Rev Med Pharmacol Sci 2012;16 Suppl 2:73-8. [PubMed]


