South Korean degenerative spondylolisthesis patients had surgical treatment at earlier age than Japanese, American, and European patients: a published literature observation
The epidemiology of lumbar degenerative spondylolisthesis (DS) has been controversial. We recently performed a systemic review with the aim to have a better understanding of DS’s prevalence in general population. The results showed the prevalence of DS is very gender specific and age specific (1). Both women and men have few DS before 50 years old, after 50 years old both women and men start to develop DS, with women having a faster developing rate than men. For elderly Chinese (mean age, 72.5 years), DS prevalence is around 25.0% for women and 19.1% for men, and the prevalence women:men ratio is 1.3:1. Elderly Caucasian American may have a higher DS prevalence, being approximately 60–70% higher than elderly Chinese; however the prevalence women:men ratio was similar to elderly Chinese population (1).
The majority of symptomatic DS patients are successfully treated without surgery. Physical therapy is the first line of treatment for adults with symptoms from spondylolisthesis. Hamstring stretching, trunk strengthening, and avoidance of inciting activities are beneficial for adults. Surgical management is offered when nonoperative options have not adequately relieved symptoms. Patients for whom surgery is indicated usually have good outcomes. Young patients may require only a fusion in situ; however, patients who have evidence of neural compression may need a decompression to relieve symptoms, and fusion is usually also indicated in these cases (2,3).
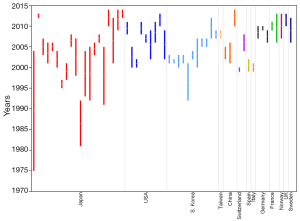
In our last study (1), preliminary data showed the ratio of numbers of female patients received treatment compared with men did not differ between Northeast Asians (Chinese, Japanese, and Korean) and European and American Caucasians, being around 2:1 in elderly population. However, compared with Caucasians, Asians were likely to have surgical treatment more than half decade earlier (1). We were interested whether it was due to Northeast Asians manifest clinical symptoms earlier or more severe, and therefore did this further literature analysis. We used the PubMed search results we obtained for our last paper (1). To broadly include data, only the word ‘spondylolisthesis’ was used for search, and updated till September 18, 2016. We selected original research data involving surgical treatment of DS and published after year 2000, and reported from Japan [n=37 series, references (4-28)], South Korea [n=11, references (29-38)], mainland China [n=5 series, references (39-41)], and Taiwan [n=3 series, references (42,43)], America [(n=20 series, references (44-56)], and Europe [n=23 series, references (57-72)]. With the publications used for this analysis, European countries included Germany, United Kingdom, France, Italy, Spain, Sweden, Switzerland, and Norway. The mean ages of each patient series reported were extracted and used a single entry (Figure 1). We tried our best to filter double/multiple reported data. It was noted that the series reported from mainland China often contain both congenital spondylolisthesis and DS. This lead to only five series could be used in this analysis.
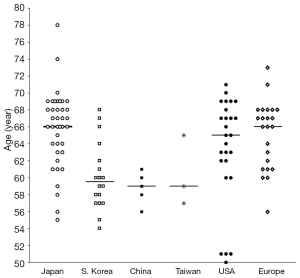
The pooled results show median age of DS patients underwent surgical treatment was 66 years for Japan, 60 years for South Korea, 59 years for mainland China, 59 years for Taiwan, 65 years for USA, and 66 years for Europe (Figure 1). The median age of DS patients underwent surgical treatment in Japan, USA, and Europe was similar; while that of South Korea, mainland China, and maybe also Taiwan, was younger. The surgery dates in the reports (Figure 2) [Japan (4-28), South Korea (29-38), mainland China (39-41), and Taiwan (42,43), America (44-56), Europe (57-72)] suggest the patient age differences between South Korea, Japan, USA, and Europe were unlikely caused by the difference of the year of operations.
This study represents a limited observation of published literatures. We did not perform statistical analysis, we also did not add weighting factor to each patient series according to study subject number. However, we believe the trend we saw in this study is likely to be real. This study indicates Japan and South Korea may have different surgical practice patterns. Our previous observation that Northeast Asians probably had surgical treatment earlier than Caucasians was likely not due to Northeast Asians manifest clinical symptoms earlier or more severe because of ethnic difference (1). Instead, it was mainly due to DS patients in South Korea and China were more likely to undergo treatment at earlier age. It will be of interests to investigate whether more proportions of DS patients have been treated surgically in South Korea than in Japan. The cost-effectiveness of different approaches may require further analysis by professional spine surgeons.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wang YX, Kaplar Z, Deng M, Leung J. Lumbar degenerative spondylolisthesis epidemiology: a systemic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat 2016. [Epub ahead of print].
- Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. Instr Course Lect 2008;57:431-45. [PubMed]
- North American Spine Society. Evidence-based clinical guidelines for multidisciplinary spine care. Diagnosis and treatment of degenerative lumbar spondylolisthesis. 2nd edition. Burr Ridge, IL 60527, USA: North American Spine Society, 2014. Available online: https://www.spine.org/documents/researchclinicalcare/guidelines/spondylolisthesis.pdf
- Tsuji T, Watanabe K, Hosogane N, Fujita N, Ishii K, Chiba K, Toyama Y, Nakamura M, Matsumoto M. Risk factors of radiological adjacent disc degeneration with lumbar interbody fusion for degenerative spondylolisthesis. J Orthop Sci 2016;21:133-7. [Crossref] [PubMed]
- Oishi Y, Murase M, Hayashi Y, Ogawa T, Hamawaki J. Smaller facet effusion in association with restabilization at the time of operation in Japanese patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine 2010;12:88-95. [Crossref] [PubMed]
- Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Fujimoto K, Shiga Y, Abe K, Kanamoto H, Inoue G, Takahashi K. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Ikuta K, Tono O, Oga M. Clinical outcome of microendoscopic posterior decompression for spinal stenosis associated with degenerative spondylolisthesis--minimum 2-year outcome of 37 patients. Minim Invasive Neurosurg 2008;51:267-71. [Crossref] [PubMed]
- Tsutsumimoto T, Shimogata M, Ohta H, Misawa H. Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis: comparison of paraspinal muscle damage and slip reduction. Spine 2009;34:1923-8. [Crossref] [PubMed]
- Sasai K, Umeda M, Maruyama T, Wakabayashi E, Iida H. Microsurgical bilateral decompression via a unilateral approach for lumbar spinal canal stenosis including degenerative spondylolisthesis. J Neurosurg Spine 2008;9:554-9. [Crossref] [PubMed]
- Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J 2008;17:1107-12. [Crossref] [PubMed]
- Matsudaira K, Yamazaki T, Seichi A, Takeshita K, Hoshi K, Kishimoto J, Nakamura K. Spinal stenosis in grade I degenerative lumbar spondylolisthesis: a comparative study of outcomes following laminoplasty and laminectomy with instrumented spinal fusion. J Orthop Sci 2005;10:270-6. [Crossref] [PubMed]
- Mori G, Mikami Y, Arai Y, Ikeda T, Nagae M, Tonomura H, Takatori R, Sawada K, Fujiwara H, Kubo T. Outcomes in cases of lumbar degenerative spondylolisthesis more than 5 years after treatment with minimally invasive decompression: examination of pre- and postoperative slippage, intervertebral disc changes, and clinical results. J Neurosurg Spine 2016;24:367-74. [Crossref] [PubMed]
- Sakaura H, Yamashita T, Miwa T, Ohzono K, Ohwada T. Outcomes of 2-level posterior lumbar interbody fusion for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine 2013;19:90-4. [Crossref] [PubMed]
- Dohzono S, Matsumura A, Terai H, Toyoda H, Suzuki A, Nakamura H. Radiographic evaluation of postoperative bone regrowth after microscopic bilateral decompression via a unilateral approach for degenerative lumbar spondylolisthesis. J Neurosurg Spine 2013;18:472-8. [Crossref] [PubMed]
- Ohtori S, Koshi T, Yamashita M, Takaso M, Yamauchi K, Inoue G, Suzuki M, Orita S, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Ishikawa T, Arai G, Miyagi M, Kamoda H, Suzuki M, Nakamura J, Furuya T, Toyone T, Yamagata M, Takahashi K. Single-level instrumented posterolateral fusion versus non-instrumented anterior interbody fusion for lumbar spondylolisthesis: a prospective study with a 2-year follow-up. J Orthop Sci 2011;16:352-8. [Crossref] [PubMed]
- Kanamori M, Yasuda T, Hori T, Suzuki K, Kawaguchi Y. Minimum 10-Year Follow-up Study of Anterior Lumbar Interbody Fusion for Degenerative Spondylolisthesis: Progressive Pattern of the Adjacent Disc Degeneration. Asian Spine J 2012;6:105-14. [Crossref] [PubMed]
- Ito Y, Oda H, Taguchi T, Inoue H, Kawai S. Results of surgical treatment for lumbar canal stenosis due to degenerative spondylolisthesis: enlargement of the lumbar spinal canal. J Orthop Sci 2003;8:648-56. [Crossref] [PubMed]
- Hosono N, Namekata M, Makino T, Miwa T, Kaito T, Kaneko N, Fuji T. Perioperative complications of primary posterior lumbar interbody fusion for nonisthmic spondylolisthesis: analysis of risk factors. J Neurosurg Spine 2008;9:403-7. [Crossref] [PubMed]
- Sasaki O, Nakamura K, Nashimoto T, Yamashita S, Yajima N, Suzuki K, Saito A. Long-term results of decompressive surgery without fusion for degenerative spondylolisthesis. No Shinkei Geka 2014;42:1109-17. [PubMed]
- Funao H, Tsuji T, Hosogane N, Watanabe K, Ishii K, Nakamura M, Chiba K, Toyama Y, Matsumoto M. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J 2012;21:2181-7. [Crossref] [PubMed]
- Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, Nakajima A, Toyone T, Orita S, Takahashi K. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages. J Neurosurg Spine 2012;17:153-9. [Crossref] [PubMed]
- Nakanishi K, Tanaka N, Fujimoto Y, Okuda T, Kamei N, Nakamae T, Izumi B, Ohta R, Fujioka Y, Ochi M. Medium-term clinical results of microsurgical lumbar flavectomy that preserves facet joints in cases of lumbar degenerative spondylolisthesis: comparison of bilateral laminotomy with bilateral decompression by a unilateral approach. J Spinal Disord Tech 2013;26:351-8. [Crossref] [PubMed]
- Kotani Y, Abumi K, Ito M, Sudo H, Abe Y, Minami A. Mid-term clinical results of minimally invasive decompression and posterolateral fusion with percutaneous pedicle screws versus conventional approach for degenerative spondylolisthesis with spinal stenosis. Eur Spine J 2012;21:1171-7. [Crossref] [PubMed]
- Ikuta K, Masuda K, Tominaga F, Sakuragi T, Kai K, Kitamura T, Senba H, Shidahara S. Clinical and Radiological Study Focused on Relief of low Back Pain Following Decompression Surgery in Selected Patients of Lumbar Spinal Stenosis Associated with Grade I Degenerative Spondylolisthesis. Spine 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Posterior lumbar interbody fusion with cortical bone trajectory screw fixation versus posterior lumbar interbody fusion using traditional pedicle screw fixation for degenerative lumbar spondylolisthesis: a comparative study. J Neurosurg Spine 2016;25:591-5. [Crossref] [PubMed]
- Inui T, Murakami M, Nagao N, Miyazaki K, Matsuda K, Tominaga Y, Kitano M, Hasegawa H, Tominaga S. Lumbar Degenerative Spondylolisthesis: Changes in Surgical Indications and Comparison of Instrumented Fusion with Two Surgical Decompression Procedures. Spine (Phila Pa 1976) 2017;42:E15-E24. [Crossref] [PubMed]
- Ninomiya K, Iwatsuki K, Ohnishi Y, Yoshimine T. Radiological Evaluation of the Initial Fixation between Cortical Bone Trajectory and Conventional Pedicle Screw Technique for Lumbar Degenerative Spondylolisthesis. Asian Spine J 2016;10:251-7. [Crossref] [PubMed]
- Mori K, Nishizawa K, Nakamura A, Imai S. Short-Term Clinical Result of Cortical Bone Trajectory Technique for the Treatment of Degenerative Lumbar Spondylolisthesis with More than 1-Year Follow-Up. Asian Spine J 2016;10:238-44. [Crossref] [PubMed]
- Lee SH, Lee JH, Hong SW, Chung SE, Yoo SH, Lee HY. Spinopelvic alignment after interspinous soft stabilization with a tension band system in grade 1 degenerative lumbar spondylolisthesis. Spine 2010;35:E691-701. [Crossref] [PubMed]
- Hong SW, Lee HY, Kim KH, Lee SH. Interspinous ligamentoplasty in the treatment of degenerative spondylolisthesis: midterm clinical results. J Neurosurg Spine 2010;13:27-35. [Crossref] [PubMed]
- Shim CS, Lee SH, Park SH, Whang JH. Soft stabilization with an artificial intervertebral ligament in grade I degenerative spondylolisthesis: comparison with instrumented posterior lumbar interbody fusion. SAS J 2007;1:118-24. [Crossref] [PubMed]
- Kim KH, Lee SH, Shim CS, Lee DY, Park HS, Pan WJ, Lee HY. Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4-L5 spondylolisthesis: a minimum five-year follow-up. Spine 2010;35:625-34. [Crossref] [PubMed]
- Ha KY, Na KH, Shin JH, Kim KW. Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech 2008;21:229-34. [Crossref] [PubMed]
- Lee SH, Lee JH, Hong SW, Shim CS, Chung SE, Yoo SH, Lee HY. Factors affecting clinical outcomes in treating patients with grade 1 degenerative spondylolisthesis using interspinous soft stabilization with a tension band system: a minimum 5-year follow-up. Spine 2012;37:563-72. [Crossref] [PubMed]
- Yu CH, Lee JE, Yang JJ, Chang BS, Lee CK. Adjacent Segment Degeneration after Single-Level PLIF: Comparison between Spondylolytic Spondylolisthesis, Degenerative Spondylolisthesis and Spinal Stenosis. Asian Spine J 2011;5:82-90. [Crossref] [PubMed]
- Jang JW, Park JH, Hyun SJ, Rhim SC. Clinical Outcomes and Radiologic Changes After Microsurgical Bilateral Decompression by a Unilateral Approach in Patients With Lumbar Spinal Stenosis and Grade I Degenerative Spondylolisthesis With a Minimum 3-Year Follow-Up. Clin Spine Surg 2016;29:268-71. [PubMed]
- Park JH, Hyun SJ, Roh SW, Rhim SC. A comparison of unilateral laminectomy with bilateral decompression and fusion surgery in the treatment of grade I lumbar degenerative spondylolisthesis. Acta Neurochir (Wien) 2012;154:1205-12. [Crossref] [PubMed]
- Park Y, Ha JW, Lee YT, Oh HC, Yoo JH, Kim HB. Surgical outcomes of minimally invasive transforaminal lumbar interbody fusion for the treatment of spondylolisthesis and degenerative segmental instability. Asian Spine J 2011;5:228-36. [Crossref] [PubMed]
- Yan DL, Pei FX, Li J, Soo CL. Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 2008;17:1311-6. [Crossref] [PubMed]
- Xu H, Tang H, Li Z. Surgical treatment of adult degenerative spondylolisthesis by instrumented transforaminal lumbar interbody fusion in the Han nationality. J Neurosurg Spine 2009;10:496-9. [Crossref] [PubMed]
- Fan G, Zhang H, Guan X, Gu G, Wu X, Hu A, Gu X, He S. Patient-reported and radiographic outcomes of minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis with or without reduction: A comparative study. J Clin Neurosci 2016;33:111-8. [Crossref] [PubMed]
- Kuo CH, Chang PY, Wu JC, Chang HK, Fay LY, Tu TH, Cheng H, Huang WC. Dynamic stabilization for L4-5 spondylolisthesis: comparison with minimally invasive transforaminal lumbar interbody fusion with more than 2 years of follow-up. Neurosurg Focus 2016;40:E3. [Crossref] [PubMed]
- Fay LY, Wu JC, Tsai TY, Wu CL, Huang WC, Cheng H. Dynamic stabilization for degenerative spondylolisthesis: evaluation of radiographic and clinical outcomes. Clin Neurol Neurosurg 2013;115:535-41. [Crossref] [PubMed]
- Eliades P, Rahal JP, Herrick DB, Corliss BM, Riesenburger R, Hwang S, Kryzanski JT. Unilateral Pedicle Screw Fixation is Associated with Reduced Cost and Similar Outcomes in Selected Patients Undergoing Minimally Invasive Transforaminal Lumbar Interbody Fusion for L4-5 Degenerative Spondylolisthesis. Cureus 2015;7:e249. [PubMed]
- Abdu WA, Lurie JD, Spratt KF, Tosteson AN, Zhao W, Tosteson TD, Herkowitz H, Longely M, Boden SD, Emery S, Weinstein JN. Degenerative spondylolisthesis: does fusion method influence outcome? Four-year results of the spine patient outcomes research trial. Spine 2009;34:2351-60. [Crossref] [PubMed]
- Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X STOP device in patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine 2006;4:463-71. [Crossref] [PubMed]
- Ghogawala Z, Benzel EC, Amin-Hanjani S, Barker FG 2nd, Harrington JF, Magge SN, Strugar J, Coumans JV, Borges LF. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative Grade I spondylolisthesis. J Neurosurg Spine 2004;1:267-72. [Crossref] [PubMed]
- Ahmadian A, Verma S, Mundis GM Jr, Oskouian RJ Jr, Smith DA, Uribe JS. Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: clinical outcomes. J Neurosurg Spine 2013;19:314-20. [Crossref] [PubMed]
- Agabegi SS, Majid K, Fischgrund JS, Vaccaro AR, Patel T. Can preoperative radiographic parameters be used to predict fusion in non-instrumented posterolateral fusion for degenerative spondylolisthesis? Spine 2011;36:E1709-14. [Crossref] [PubMed]
- Adogwa O, Parker SL, Davis BJ, Aaronson O, Devin C, Cheng JS, McGirt MJ. Cost-effectiveness of transforaminal lumbar interbody fusion for Grade I degenerative spondylolisthesis. J Neurosurg Spine 2011;15:138-43. [Crossref] [PubMed]
- Parker SL, Adogwa O, Bydon A, Cheng J, McGirt MJ. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg 2012;78:178-84. [Crossref] [PubMed]
- Davis R, Auerbach JD, Bae H, Errico TJ. Low-grade spondylolisthesis be effectively treated by either coflex interlaminar stabilization or laminectomy and posterior spinal fusion? Two-year clinical and radiographic results from the randomized, prospective, multicenter US investigational device exemption trial: clinical article. J Neurosurg Spine 2013;19:174-84. [Crossref] [PubMed]
- Blumenthal C, Curran J, Benzel EC, Potter R, Magge SN, Harrington JF Jr, Coumans JV, Ghogawala Z. Radiographic predictors of delayed instability following decompression without fusion for degenerative grade I lumbar spondylolisthesis. J Neurosurg Spine 2013;18:340-6. [Crossref] [PubMed]
- Rodgers WB, Lehmen JA, Gerber EJ, Rodgers JA. Grade 2 spondylolisthesis at L4-5 treated by XLIF: safety and midterm results in the "worst case scenario". ScientificWorldJournal 2012;2012:356712.
- Snoddy MC, Sielatycki JA, Sivaganesan A, Engstrom SM, McGirt MJ, Devin CJ. Can facet joint fluid on MRI and dynamic instability be a predictor of improvement in back pain following lumbar fusion for degenerative spondylolisthesis? Eur Spine J 2016;25:2408-15. [Crossref] [PubMed]
- Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC. Laminectomy plus Fusion versus Laminectomy Alone for Lumbar Spondylolisthesis. N Engl J Med 2016;374:1424-34. [Crossref] [PubMed]
- Lara-Almunia M, Gomez-Moreta JA, Hernandez-Vicente J. Posterior lumbar interbody fusion with instrumented posterolateral fusion in adult spondylolisthesis: description and association of clinico-surgical variables with prognosis in a series of 36 cases. Int J Spine Surg 2015;9:22. [PubMed]
- Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery 2007;61:981-6; discussion 986. [Crossref] [PubMed]
- Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine 2008;33:E636-42. [Crossref] [PubMed]
- Fernández-Fairen M, Sala P, Ramírez H, Gil J. A prospective randomized study of unilateral versus bilateral instrumented posterolateral lumbar fusion in degenerative spondylolisthesis. Spine 2007;32:395-401. [Crossref] [PubMed]
- Gaetani P, Aimar E, Panella L, Levi D, Tancioni F, Di Ieva A, Debernardi A, Pisano P, Rodriguez y Baena R. Functional disability after instrumented stabilization in lumbar degenerative spondylolisthesis: a follow-up study. Funct Neurol 2006;21:31-7. [PubMed]
- Wegmann K, Gundermann S, Siewe J, Eysel P, Delank KS, Sobottke R. Correlation of reduction and clinical outcome in patients with degenerative spondylolisthesis. Arch Orthop Trauma Surg 2013;133:1639-44. [Crossref] [PubMed]
- Boon Tow BP, Yue WM, Srivastava A, Lai JM, Guo CM, Wearn Peng BC, Chen JL, Yew AK, Seng C, Tan SB. Does Navigation Improve Accuracy of Placement of Pedicle Screws in Single-level Lumbar Degenerative Spondylolisthesis?: A Comparison Between Free-hand and Three-dimensional O-Arm Navigation Techniques. J Spinal Disord Tech 2015;28:E472-7. [Crossref] [PubMed]
- Archavlis E, Carvi y Nievas M. Comparison of minimally invasive fusion and instrumentation versus open surgery for severe stenotic spondylolisthesis with high-grade facet joint osteoarthritis. Eur Spine J 2013;22:1731-40. [Crossref] [PubMed]
- Kleinstueck FS, Fekete TF, Mannion AF, Grob D, Porchet F, Mutter U, Jeszenszky D. To fuse or not to fuse in lumbar degenerative spondylolisthesis: do baseline symptoms help provide the answer? Eur Spine J 2012;21:268-75. [Crossref] [PubMed]
- Klessinger S. Radiofrequency neurotomy for treatment of low back pain in patients with minor degenerative spondylolisthesis. Pain Physician 2012;15:E71-8. [PubMed]
- Challier V, Boissiere L, Obeid I, Vital JM, Castelain JE, Bénard A, Ong N, Ghailane S, Pointillart V, Mazas S, Mariey R, Gille O. One-Level Lumbar Degenerative Spondylolisthesis And Posterior Approach. Is Transforaminal Lateral Interbody Fusion Mandatory? A Randomized Controlled Trial With Two Year Follow-Up. Spine (Phila Pa 1976) 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Kitchen WJ, Mohamed M, Bhojak M, Wilby M. Neurogenic claudication secondary to degenerative spondylolisthesis: is fusion always necessary? Br J Neurosurg 2016;30:662-5. [Crossref] [PubMed]
- Austevoll IM, Gjestad R, Brox JI, Solberg TK, Storheim K, Rekeland F, Hermansen E, Indrekvam K, Hellum C. The effectiveness of decompression alone compared with additional fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a pragmatic comparative non-inferiority observational study from the Norwegian Registry for Spine Surgery. Eur Spine J 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Ahmad S, Hamad A, Bhalla A, Turner S, Balain B, Jaffray D. The outcome of decompression alone for lumbar spinal stenosis with degenerative spondylolisthesis. Eur Spine J 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Moreau PE, Ferrero E, Riouallon G, Lenoir T, Guigui P. Radiologic adjacent segment degeneration 2 years after lumbar fusion for degenerative spondylolisthesis. Orthop Traumatol Surg Res 2016;102:759-63. [Crossref] [PubMed]
- Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B. A. Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis. N Engl J Med 2016;374:1413-23. [Crossref] [PubMed]