Development of a plain radiograph requesting algorithm for patients presenting with acute abdominal pain
Introduction
Radiologists at a large teaching hospital felt plain radiograph imaging was being performed inappropriately for patients admitted with acute abdominal pain. They felt a proportion of requests were either not indicated or CT was a more appropriate first line radiological investigation in certain circumstances.
This project aimed to establish whether plain radiograph imaging was being used appropriately for patients presenting with acute abdominal pain. Following the results of this audit, the next aim was to establish an algorithm to improve plain radiograph requesting and to increase the use of earlier CT where appropriate.
The initial objective was to conduct an audit, comparing plain radiograph imaging requests to Royal College of Radiologists (RCR) guidelines and establish how many patients undergoing plain radiograph imaging proceeded to CT imaging within forty-eight hours. Following the results of this audit, a second objective was to produce an algorithm for plain radiograph imaging requesting in patients presenting with acute abdominal pain. This aimed to improve plain radiograph imaging requests, to expedite use of CT following specific plain radiograph findings and to increase the requesting of CT as the first line investigation in appropriate scenarios. The final objective was to establish whether the algorithm was appropriate for implementation through presentation at local and regional clinical governance meetings.
Materials and methods
The audit was performed on plain radiograph imaging requests on an adult general surgical admissions unit (SAU) in a large teaching hospital. Data was collected by searching CRIS for plain radiograph imaging requests by the department of general surgery on the SAU in the month of August 2011. There was no limitation on the age or sex of the patient. Requests made under the department of general surgery which were not for surgical indications, such as chest radiograph requests for medical indications and limb radiographs to identify fractures, were excluded. Once a list of radiographs was collaborated, they were randomised and the first 50 requests were audited. These covered requests at all times of day, including out of hours. Audit criteria were taken from RCR referral guidelines (1). From these guidelines, indications were selected by identifying clinical/diagnostic problems in the context of acute abdominal pain indicating an investigation with a recommendation [grade] of A, B or C. These include (specifically as described by the referral guidelines):
- Acute abdominal pain; obstruction/perforation;
- Suspected esophageal perforation;
- Acute small bowel obstruction: confirmation and assessment of level;
- Acute large bowel obstruction;
- Inflammatory bowel disease (in the context of identifying toxic megacolon);
- Acute pancreatitis (only in the context of nonspecific acute abdominal pain to exclude other causes).
The 50 plain radiograph requests were then audited against these RCR referral guidelines, with a target of 100%. They were also examined to see how many of these patients proceeded to CT imaging within forty eight hours of plain radiograph imaging.
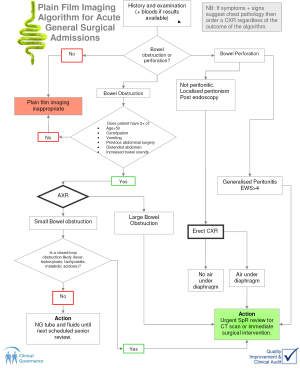
Following the results of this audit, a plain radiograph requesting algorithm was created which would potentially improve plain radiograph imaging requesting (Figure 1). The initial intention was for the algorithm to be used as a guide by junior doctors, especially out of hours where senior advice is less available. The algorithm aimed not only to ensure plain radiograph requests met RCR guidelines but also to ensure that suspected diagnoses indicating the plain radiograph were likely, through the use of specific clinical parameters. A second aim was to increase the use of CT as the initial radiological investigation where appropriate and to expedite the use of CT following specific plain radiograph findings. Overall, this algorithm would hopefully reduce unnecessary radiation exposure by reducing plain radiographs which are not indicated and improve patient care by identifying diagnoses earlier through the appropriate use of earlier CT. The major difficulty in the creation of the algorithm was finding studies which had used specific clinical criterion to diagnose abdominal obstruction or perforation (the major two indications for plain film imaging in acute abdominal pain), thus indicating the need for plain radiograph or CT. Furthermore, there was little in the literature examining at which stage CT is appropriate in a patient presenting with possible obstruction or perforation.
The first step in the algorithm creation was to exclude plain film imaging requests which were not for suspected bowel obstruction or perforation, following the history and examination (and blood results if available). The algorithm then split into that for suspected bowel obstruction and that for perforation.
For suspected bowel obstruction, the literature was searched using pubMed for articles which used ‘history and examination findings to identify suspected bowel obstruction’. The most relevant study calculated the sensitivity, specificity, positive predictive value and negative predictive value for 45 pre-imaging variables in the diagnosis of bowel obstruction (2). The study found that combining two of the most common six symptoms of diagnostic help (distended abdomen, increased bowel sounds, constipation, previous abdominal surgery, age over 50 and vomiting) significantly improved sensitivity. They created an algorithm and retrospectively found that if ‘two out of six symptoms’ had been applied, then 42% of plain films could have been avoided with only 2.1% cases bowel obstruction missed. This was then placed into the algorithm.
If the scenario met two out of the six criteria then the next step was to perform an abdominal radiograph. If the findings showed large bowel obstruction then there needed to be an urgent surgical specialist registrar (SpR) review for consideration of urgent CT or to proceed straight to surgery. If the radiograph showed small bowel obstruction then the key factor was whether high grade (complete) or low grade small bowel obstruction was likely, as high grade obstruction warranted urgent action. The literature was lacking in specific clinical variables to differentiate high grade from low grade obstruction. One article identified that fever, leukocytosis, metabolic acidosis and tachycardia were the most useful markers of high grade obstruction warranting explorative surgery in patients with confirmed small bowel obstruction (3). These parameters were then placed into the algorithm. If present then urgent Surgical SpR review with consideration of CT or explorative surgery was required. If not present then symptomatic management until the next scheduled senior review was appropriate (usually involving placement of naso-gastric tube for aspiration and intra-venous fluids with appropriate electrolyte replacement). This completed the ‘bowel obstruction’ part of the algorithm.
If bowel perforation was suspected then it needed to be decided whether localised or generalised peritonitis was present. Due to a lack of literature determining whether clinical parameters could differentiate between the two, the algorithm group made a decision based on previous clinical experience. Localised peritonism was thought to be present if no physical signs of peritonism were present (but perforation still suspected), if physical examination revealed localised peritonism or if the patient was post endoscopy. In this scenario, an erect chest radiograph was appropriate. If there was no free air under the diaphragm then, from an imaging perspective, the patient could wait until the next scheduled senior review to decide on further investigation. If free air was under the diaphragm, then an urgent surgical SpR review was warranted with a view to either urgent CT or surgery. Generalised peritonitis was to be suspected if there were signs of generalised peritonitis on examination, or if the early warning score (EWS) was greater than 4. This required urgent surgical SpR review with a view to either CT or urgent surgery.
Results
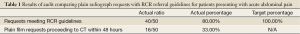
The results of the audit were as follows. 80% (40/50) plain radiograph requests did not meet RCR guidelines, meaning 20% of requests were not indicated (Table 1). 33% (16/50) patients with acute abdominal pain who had a plain film performed proceeded to CT within 48 hours.
Full table
Discussion
The results of this audit demonstrated that 20% plain film imaging requests failed to meet RCR guidelines, and are therefore unnecessary. Another observation by general surgical consultants was that occasionally, junior doctors used recognised indications (e.g., bowel obstruction) for plain radiograph requests where actually these diagnoses where unlikely. This suggests that the number of non indicated plain radiographs is potentially higher. The objective auditing of this issue was beyond the scope of this project, but, as described in the methods section, the algorithm attempted to address this through the use of specific parameters. The audit also identified that one third of patients undergoing plain film imaging proceeded to CT within forty eight hours, suggesting the need for earlier CT, or using CT as the initial investigation in these patients.
The annual volume and cost of plain film imaging for the general surgical department on the SAU was calculated; 2,270 plain films were performed at an annual cost of £36,320. Based on this audit, 20-50% plain abdominal radiographs were either inappropriate or CT would be a more appropriate first line investigation. Therefore the SAU could potentially reduce the number of plain films by 454-1,135 per year with an annual saving of £7,264- £18,160. The algorithm was then created as described in the methods section. It should be mentioned that whilst there were likely to be savings from reducing plain film imaging, the algorithm would likely increase the more expensive modality of CT and thus overall cost would increase. However, if this reduced time to diagnosis, thereby reducing patient morbidity and inpatient stay, then overall patient benefit would improve. The analysis of cost comparison in this respect was beyond the scope of this audit.
The audit and algorithm was then discussed at local and regional clinical governance meetings. The local clinical governance meeting addressed general surgical issues only, with general surgical trainees and consultants present. The regional audit meeting addressed issues from a range of specialties and there were consultants present from general surgery, internal medicine and anaesthetics. The overall view of the general surgical consultants was as follows:
(I) Earlier CT would be beneficial to patients in terms of earlier diagnoses and reducing patient stay in specific circumstances. The algorithm provides a good framework for expediting CT appropriately in acute abdominal pain admissions with suspected bowel obstruction or perforation.
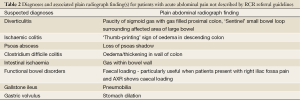
(II) Plain radiographs are useful for general surgical admissions presenting with acute abdominal pain with suspected diagnoses outside those indicated by the RCR. Whilst the plain abdominal radiograph may not be the principal diagnostic modality for many general surgical diagnoses, it can reveal findings associated with these diagnoses. When this has been coupled with the history, examination and blood results then a likely diagnoses can made by experienced clinicians, avoiding the need for further imaging or explorative surgery. Table 2 gives the full list of the potential diagnoses and their respective plain radiograph findings outside RCR indications which were discussed at the meetings. An example of a plain radiograph finding not described by RCR guidelines is the paucity of sigmoid gas with gas filled proximal colon in diverticulitis.
Full table
Conclusions
CT continues to become an increasingly common imaging technique in the diagnoses of patients presenting with acute abdominal pain, prior to patients undergoing surgery. If used appropriately, there are clear benefits to this as patients benefit from earlier diagnoses, potentially avoid complications by earlier intervention and avoid the need for explorative surgery as CT confirms or excludes the suspected diagnosis. This algorithm provides a framework for junior doctors making imaging decisions in patients with suspected obstruction or perforation; particularly useful out of hours where senior advice is less available. It is difficult to create a national or international algorithm for plain radiograph imaging requests in patients presenting with acute abdominal pain as each hospital/trust has different access to different expertise and imaging modalities. The algorithm developed in this project could act as a model which could be adapted according to the resources of an individual hospital. Following outcome at the general surgical clinical governance meeting, there are plans to change the initial step in this plain film requesting algorithm. However, the feeling was that the steps to expediting CT scanning in suspected bowel obstruction or perforation were useful, especially for junior doctors making imaging decisions out of hours.
Whilst the plain abdominal radiograph may be the principal diagnostic imaging modality for only a small number of suspected diagnoses in acute abdominal pain, it can reveal findings associated with a broader range of diagnoses than that suggested by the RCR. When this is combined with other clinical information then diagnoses can be made by experienced clinicians, avoiding the need for CT, alternative imaging or explorative surgery. RCR should consider broadening its referral guidelines for plain radiograph imaging in acute abdominal pain. The recommendation [grade] would depend on the evidence for each diagnosis and if another principal diagnostic modality exists for that diagnosis, the plain abdominal radiograph should not replace this unless evidence suggest otherwise. However, if the plain radiograph findings for a broader range of diagnoses were added to the referral guidelines, clinicians could combine the plain radiograph findings with other clinical information to make a diagnosis, potentially avoiding the need for CT or explorative surgery, thereby reducing cost and improving overall patient care.
Acknowledgements
Dr. Andrew Longstaff. Consultant radiologist, Frenchay hospital. Suggested need for audit and helped with development of algorithm; Miss. Anne Pullyblank. Consultant general surgeon, Frenchay hospital. Helped with development of algorithm; Mr. Alan Roe. Consultant general surgeon, Frenchay hospital. Chaired clinical governance meeting where algorithm was discussed, suggested need to broaden RCR guidelines and helped with editing article.
Disclosure: There is no involvement which poses a potential conflict of interest.
References
- The Royal College of Radiologists. Making the best use of clinical radiology services; referral guidelines. London: The Royal College of Radiologists, 2007:85-103.
- Böhner H, Yang Q, Franke C, et al. Simple data from history and physical examination help to exclude bowel obstruction and to avoid radiographic studies in patients with acute abdominal pain. Eur J Surg 1998;164:777-84. [PubMed]
- Pekmezci S, Saribeyoglu K, Korman U. Guidelines for management of small bowel obstruction. J Trauma 2009;66:1262. [PubMed]