Bilateral renal lymphangiectasia—an unusual cause of abdominal distension and flank pain in a child
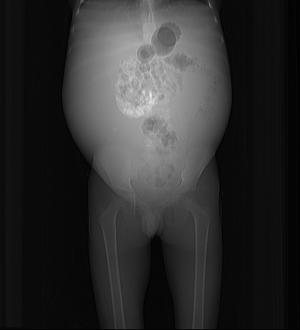
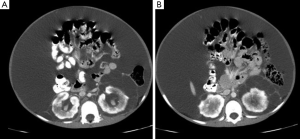
Renal lymphangiectasia (RL, also known as renal lymphangiomatosis or renal lymphangioma or parapelvic lymphangiectasia) is an uncommon benign disorder characterized by dilatation of perirenal, peripelvic and intrarenal lymphatic channels secondary to obstruction (1,2). About five cases of this entity in pediatric age group have been illustrated in literature till date (3-7). Diagnosis is based on the characteristic radiological findings. An 11-year-old male patient presented with the history of fatigue, progressively increasing abdominal distension and bilateral flank pain since last 2 months. Past history and family history was unremarkable. General physical examination including blood pressure was normal. Per abdomen examination revealed dull note on abdominal percussion suggestive of ascites. Routine laboratory investigations including complete blood profile, blood urea and serum creatinine were normal. Plain and contrast enhanced computed tomography (CECT) of abdomen was done. Topogram of CT abdomen showed diffusely increased density of abdomen with bulging flanks and poor definition of liver, spleen & psoas muscles along with the medial displacement of bowel loops (Figure 1). Plain CT axial sections of the abdomen showed septated fluid collection in bilateral perinephric and peripelvic space along with ascites (Figure 2). The septa in septated collections showed enhancement on contrast enhanced CT (Figures 3,4). The diagnosis of RL was made based on the pathognomonic imaging features. Diagnostic and therapeutic ascitic fluid tap was performed under ultrasound (US) guidance. Laboratory analysis of the fluid revealed high protein concentration with few lymphocytes. Patient was kept on the diuretics and showed significant improvement on follow-up.


The etiopathogenesis of RL, which is characterized by ectatic endothelial-lined spaces in the cortex with sparing of the medulla and with no glomerular or tubular abnormalities, is still not very clear. The lymphatic channels in the renal sinus, which connect the lymphatic system of kidneys with the renal capsule and the perirenal tissues, drain into the retroperitoneal lymph nodes. Developmental malformation of these channels is one hypothesis described to explain the origin of RL, due to the familial association seen in some cases. The other theory suggests renal/perinephric inflammation as the cause of obstruction and dilatation of lymphatics. Few suggest it as a distinct neoplastic entity (2,8,9).
Literature search on PubMed showed five cases of RL in pediatric age group. Merguerian et al. reported first case of unilateral RL in an infant in 1995 and concluded that RL should be considered as differential diagnosis of unilateral renal enlargement in children. Two years later, Simonton et al. reported another similar case of unilateral RL in a 2-year-old child presenting with hypertension, massive ascites and flank mass. Subsequently, another case was added by Cadnapaphornchai et al. in a 7-year-old child with bilateral RL presenting as renal insufficiency. Furthermore, Sanchez et al. published another case of unilateral RL in a 4-month-old female as an incidental finding. Lastly, Vasquez et al. reported a pediatric patient with bilateral RL in 2012 and emphasized the importance of identifying this pathology by characteristic radiological findings (3-7).
Most of the patients are asymptomatic and it is detected as an incidental finding on various imaging studies done for an unrelated cause. Abdominal pain, flank pain, haematuria, fatigue and weight loss are the usual presenting symptoms in symptomatic cases. Advanced cases manifest with ascites and renal insufficiency (2,10,11). The complications include renal vein thrombosis, hypertension (due to compressive effects of perirenal and peripelvic cysts causing renin-dependent arterial hypertension), superimposed infection, intracystic hemorrhage, obstructive uropathy. Partial regression during neonatal period has been described (11-15).
Imaging features on various diagnostic modalities like US, CT and magnetic resonance imaging (MRI) are classical and allow for a confident diagnosis, although, it can be further confirmed with aspiration of chylous fluid from perirenal fluid collections in cases of diagnostic dilemma. The distribution and extent of the lymphatics involved determines the imaging characteristics. Cases with involvement of just small intra-renal lymphatics are seen as mild diffuse enlargement of the kidney with no cystic space. These cases show diffusely echogenic renal parenchyma with poor corticomedullary differentiation on US and hyperintense signal in the cortex & hypointense signal in medulla with corticomedullary inversion on T2 weighted sequences of MR due to renal edema. Only peripelvic cysts are seen in cases where lymphatics in the renal sinus are involved. These peripelvic cysts with thin walls are better appreciated on US and T2 weighted sequences of MR and they may also show enhancement on T1 weighted sequences acquired after gadolinium administration. Larger cysts can cause obstruction of collecting system leading to hydronephrosis. Capsular lymphatic dilatation leads to septated perinephric fluid collections which show attenuation values of 0–10 Hounsfield units on CT. Rarely, multiple tortuous structures distended with clear fluid are seen in retroperitoneum surrounding great vessels in a linear pattern due to stasis of lymph channels. Fluid collections in peritoneal cavity or ascites are also sometimes seen. Al-Dofri et al. has also reported presence of pleural effusion in a case of RL (10). The lymphatic fluid collections in all the spaces show features of clear fluid on all the imaging modalities unless complicated by hemorrhage (11,13-18).
Differential diagnosis includes hydronephrosis, polycystic kidney disease, multiloculated cystic nephroma, urinomas, abscesses, lymphoma and nephroblastomatosis. The last two entities display features of soft tissue masses on all modalities with internal vascularity on US and enhancement on CT and MR, unlike fluid collections in cases of RL. Hydronephrosis shows distended collecting system with or without dilated ureter. Polycystic kidney disease shows multiple non-communicating cysts scattered in renal parenchyma with or without cysts in other solid organs like liver, spleen and pancreas. Multiloculated cystic nephroma is characterized by focal multiseptated cystic mass arising from kidney with claw shape of adjacent normal renal parenchyma. Urinomas and abscesses can be differentiated on the basis of proper history and imaging appearances of thick enhancing wall in abscess and contrast extravasation on delayed phase CT in urinoma (2,13,16).
No treatment is usually required in most asymptomatic patients with no complications. Nevertheless, periodic clinical and imaging follow up is recommended in all patients due to risk of complications especially renal failure and hypertension. Percutaneous aspiration of lymphatic collections is the first line of management in less severe symptomatic cases, but, the success rate is less in larger lesions with multiseptation. Laparoscopic ablation and nephrectomy are reserved for advanced complicated cases and cases with multiple recurrences (2,13,16).
RL remains an elusive disorder due to its rarity and unclear etiopathogenesis. This case emphasizes the need to be familiar with its radiological features on the various imaging modalities to allow prompt diagnosis due to its potential complications of renal vein thrombosis and hypertension and prevent misdiagnosis with close mimics like hydronephrosis, peripelvic cysts etc. This would also aid in avoiding unnecessary investigations and planning appropriate management.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Wani NA, Kosar T, Gojwari T, Qureshi UA. Perinephric fluid collections due to renal lymphangiectasia. Am J Kidney Dis 2011;57:347-51. [Crossref] [PubMed]
- Restrepo JM, Amaya JE, Sepúlveda NA, Vélez MU, Massaro M. Renal lymphangiectasia. MDCT and MRI findings. Rev Colomb Radiol 2011;22:1-8.
- Merguerian PA, Sargent SK, Dunn JL. Unilateral lymphangiectasis of the kidney: an unusual cause of renal enlargement in an infant. J Urol 1995;153:447-9. [Crossref] [PubMed]
- Simonton SC, Saltzman DA, Brennom W, Pergament M, Drake G, Sinaiko A, Priest JR. Cystic renal lymphangiectasia: a distinctive clinicopathologic entity in the pediatric age group. Pediatr Pathol Lab Med 1997;17:293-301. [Crossref] [PubMed]
- Cadnapaphornchai MA, Ford DM, Tyson RW, Lum GM. Cystic renal lymphangiectasia presenting as renal insufficiency in childhood. Pediatr Nephrol 2000;15:129-31. [Crossref] [PubMed]
- Sanchez F, Prieto JC, Koral K, Baker LA. Childhood renal lymphangiectasia. Int Braz J Urol 2008;34:772-3. [Crossref] [PubMed]
- Vasquez E, Kallen RJ, Shore RM, Lindgren BW. Pediatric renal lymphangiectasia: importance of recognition and accurate renal imaging. Urology 2012;80:434-6. [Crossref] [PubMed]
- Ramseyer LT. Case 34: renal lymphangiectasia. Radiology 2001;219:442-4. [Crossref] [PubMed]
- Pianezza ML, Mokhtassi A, Wu L. D'A Honey RJ. Case report: renal lymphangiectasia. Can J Urol 2006;13:3204-7. [PubMed]
- Al-Dofri SA. Renal lymphangiectasia presented by pleural effusion and ascites. J Radiol Case Rep 2009;3:5-10. [Crossref] [PubMed]
- Ashraf K, Raza SS, Ashraf O, Memon W, Memon A, Zubairi TA. Renal lymphangiectasia. Br J Radiol 2007;80:e117-8. [Crossref] [PubMed]
- Blanc M, Schmutz G, Belzile F, Sabbagh R. Renal lymphangiectasia presenting with hypertension and polycythemia. Can Urol Assoc J 2014;8:E163-6. [PubMed]
- de Vasconcelos RA, Pereira ES, Bauab T Jr, Valente RS. Renal lymphangiectasia: incidental finding at multislice computed tomography and literature review. Radiol Bras 2012;45:178-80. [Crossref]
- Rastogi R, Rastogi V. Computed tomographic scan in the diagnosis of bilateral renal lymphangiectasia. Saudi J Kidney Dis Transpl 2008;19:976-9. [PubMed]
- Upreti L, Dev A, Kumar Puri S. Imaging in renal lymphangiectasia: report of two cases and review of literature. Clin Radiol 2008;63:1057-62. [Crossref] [PubMed]
- Elbanna KY, Almutairi BM, Zidan AT. Bilateral renal lymphangiectasia: radiological findings by ultrasound, computed tomography, and magnetic resonance imaging. J Clin Imaging Sci 2015;5:6. [Crossref] [PubMed]
- Kumar K, Ahmad A, Singh M, Kumar A, Singh RP, Hussain M. Bilateral Renal Lymphangiectasia in a Thirty-two-Year-Old Woman. Nephrourol Mon 2014;7:e21736. [PubMed]
- Parazols F, Fournier L, Bouvier N, Pelage JP, Lobbedez T, Hurault de Ligny B. Renal lymphangiectasia, a rare case of perirenal infiltration. Nephrol Ther 2015;11:118-20. [Crossref] [PubMed]


